63 6.5 Variation in Blood Types
Created by: CK-12/Adapted by Christine Miller
Giving the Gift of Life
Did you ever donate blood? If you did, then you probably know that your blood type is an important factor in blood transfusions. People vary in the type of blood they inherit, and this determines which type(s) of blood they can safely receive in a transfusion. Do you know your blood type?
What Are Blood Types?
Blood is composed of cells suspended in a liquid called plasma. There are three types of cells in blood: red blood cells, which carry oxygen; white blood cells, which fight infections and other threats; and platelets, which are cell fragments that help blood clot. Blood type (or blood group) is a genetic characteristic associated with the presence or absence of certain molecules, called antigens, on the surface of red blood cells. These molecules may help maintain the integrity of the cell membrane, act as receptors, or have other biological functions. A blood group system refers to all of the gene(s), alleles, and possible genotypes and phenotypes that exist for a particular set of blood type antigens. Human blood group systems include the well-known ABO and Rhesus (Rh) systems, as well as at least 33 others that are less well known.
Antigens and Antibodies
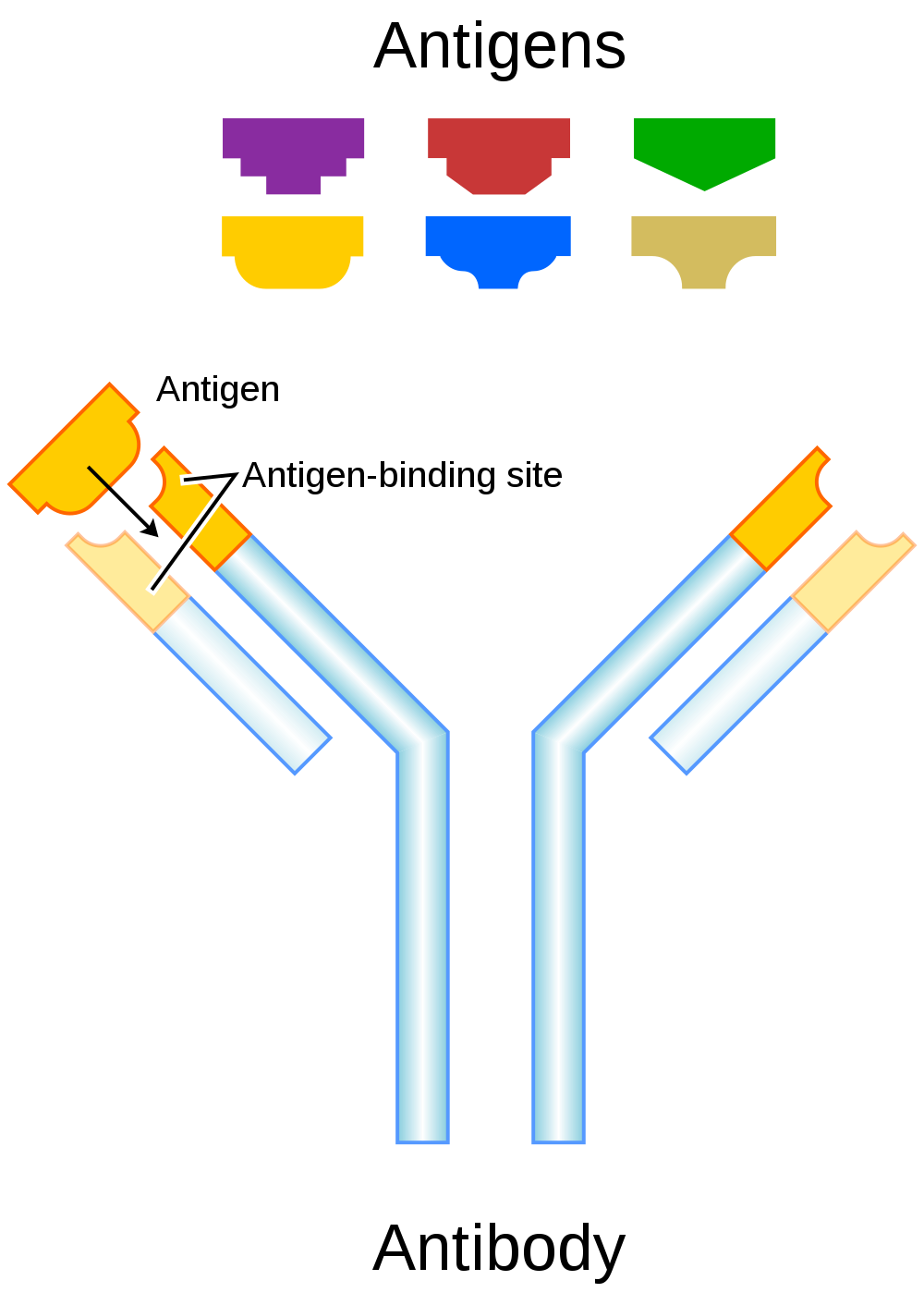
Antigens — such as those on the red blood cells — are molecules that the immune system identifies as either self (produced by your own body) or non-self (not produced by your own body). Blood group antigens may be proteins, carbohydrates, glycoproteins (proteins attached to chains of sugars), or glycolipids (lipids attached to chains of sugars), depending on the particular blood group system. If antigens are identified as non-self, the immune system responds by forming antibodies that are specific to the non-self antigens. Antibodies are large, Y-shaped proteins produced by the immune system that recognize and bind to non-self antigens. The analogy of a lock and key is often used to represent how an antibody and antigen fit together, as shown in the illustration below (Figure 6.5.2). When antibodies bind to antigens, it marks them for destruction by other immune system cells. Non-self antigens may enter your body on pathogens (such as bacteria or viruses), on foods, or on red blood cells in a blood transfusion from someone with a different blood type than your own. The last way is virtually impossible nowadays because of effective blood typing and screening protocols.
Genetics of Blood Type
An individual’s blood type depends on which alleles for a blood group system were inherited from their parents. Generally, blood type is controlled by alleles for a single gene, or for two or more very closely linked genes. Closely linked genes are almost always inherited together, because there is little or no recombination between them. Like other genetic traits, a person’s blood type is generally fixed for life, but there are rare instances in which blood type can change. This could happen, for example, if an individual receives a bone marrow transplant to treat a disease, such as leukemia. If the bone marrow comes from a donor who has a different blood type, the patient’s blood type may eventually convert to the donor’s blood type, because red blood cells are produced in bone marrow.
ABO Blood Group System
The ABO blood group system is the best known human blood group system. Antigens in this system are glycoproteins. These antigens are shown in the list below. There are four common blood types for the ABO system:
- Type A, in which only the A antigen is present.
- Type B, in which only the B antigen is present.
- Type AB, in which both the A and B antigens are present.
- Type O, in which neither the A nor the B antigen is present.
Genetics of the ABO System
The ABO blood group system is controlled by a single gene on chromosome 9. There are three common alleles for the gene, often represented by the letters A , B , and O. With three alleles, there are six possible genotypes for ABO blood group. Alleles A and B, however, are both dominant to allele O and codominant to each other. This results in just four possible phenotypes (blood types) for the ABO system. These genotypes and phenotypes are shown in Table 6.5.1.
Table 6.5.1
ABO Blood Group System: Genotypes and Phenotypes
| ABO Blood Group System | |
| Genotype | Phenotype (Blood Type, or Group) |
| AA | A |
| AO | A |
| BB | B |
| BO | B |
| OO | O |
| AB | AB |
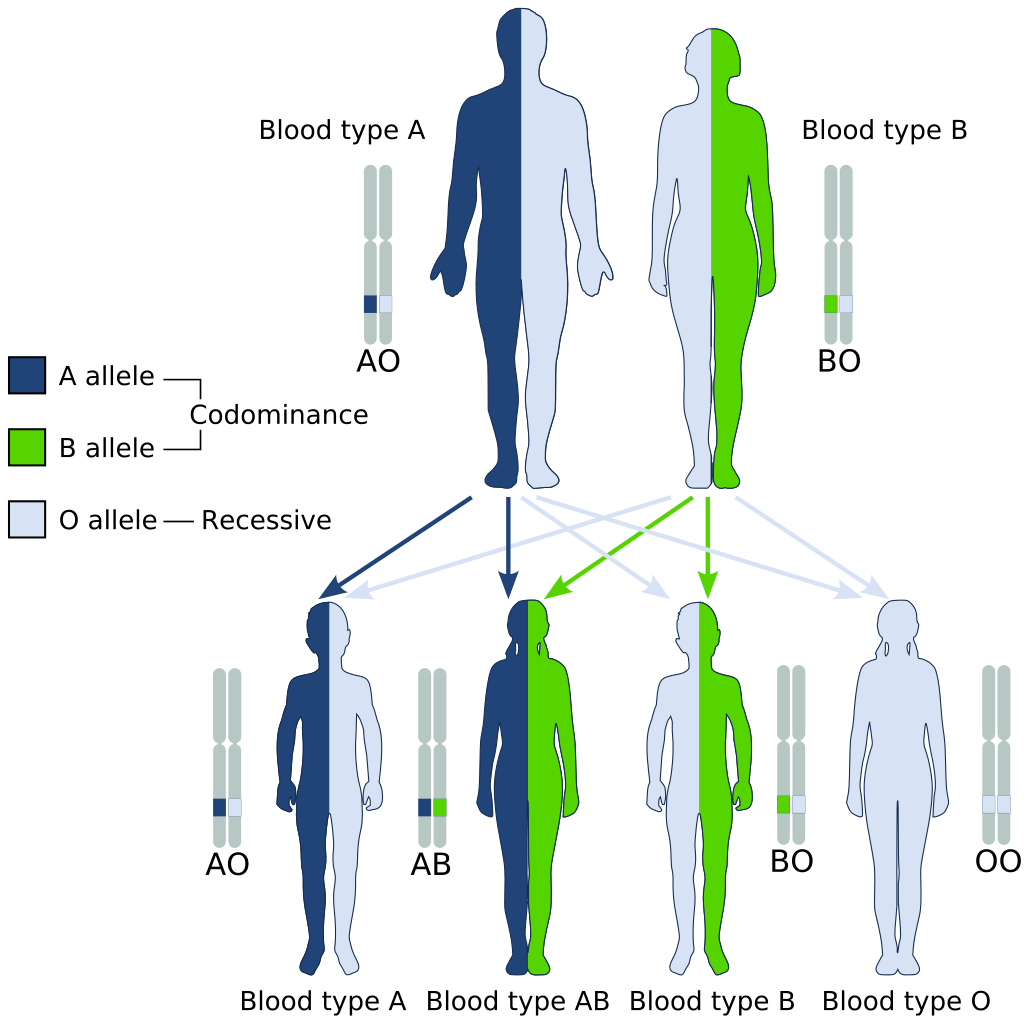
The diagram below (Figure 6.5.3) shows an example of how ABO blood type is inherited. In this particular example, the father has blood type A (genotype AO) and the mother has blood type B (genotype BO). This mating type can produce children with each of the four possible ABO phenotypes, although in any given family, not all phenotypes may be present in the children.
Medical Significance of ABO Blood Type
The ABO system is the most important blood group system in blood transfusions. If red blood cells containing a particular ABO antigen are transfused into a person who lacks that antigen, the person’s immune system will recognize the antigen on the red blood cells as non-self. Antibodies specific to that antigen will attack the red blood cells, causing them to agglutinate (or clump) and break apart. If a unit of incompatible blood were to be accidentally transfused into a patient, a severe reaction (called acute hemolytic transfusion reaction) is likely to occur, in which many red blood cells are destroyed. This may result in kidney failure, shock, and even death. Fortunately, such medical accidents virtually never occur today.
These antibodies are often spontaneously produced in the first years of life, after exposure to common microorganisms in the environment that have antigens similar to blood antigens. Specifically, a person with type A blood will produce anti-B antibodies, while a person with type B blood will produce anti-A antibodies. A person with type AB blood does not produce either antibody, while a person with type O blood produces both anti-A and anti-B antibodies. Once the antibodies have been produced, they circulate in the plasma. The relationship between ABO red blood cell antigens and plasma antibodies is shown in Figure 6.5.4.
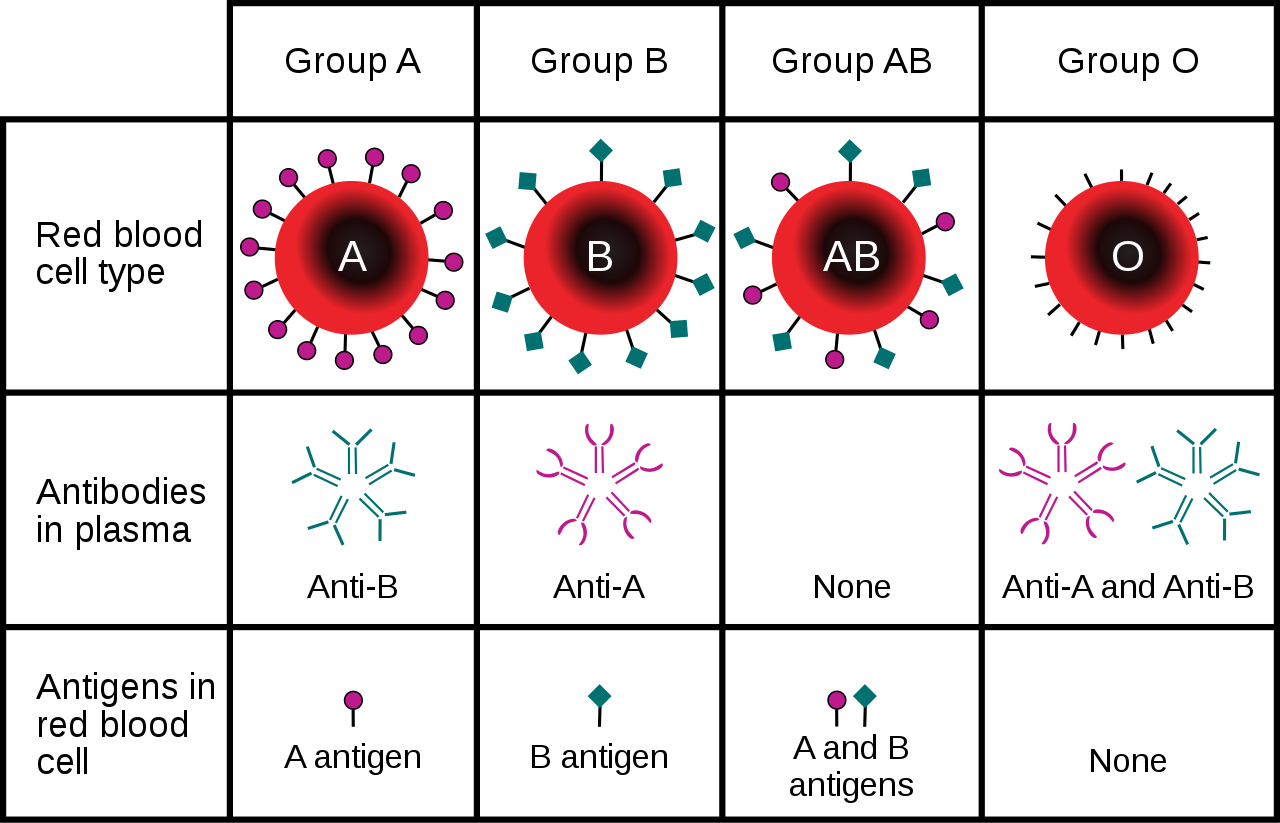
The antibodies that circulate in the plasma are for different antigens than those on red blood cells, which are recognized as self antigens.
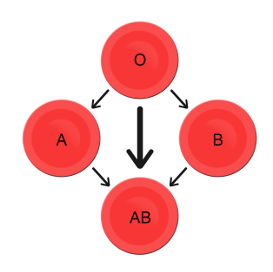
Which blood types are compatible and which are not? Type O blood contains both anti-A and anti-B antibodies, so people with type O blood can only receive type O blood. However, they can donate blood to people of any ABO blood type, which is why individuals with type O blood are called universal donors. Type AB blood contains neither anti-A nor anti-B antibodies, so people with type AB blood can receive blood from people of any ABO blood type. That’s why individuals with type AB blood are called universal recipients. They can donate blood, however, only to people who also have type AB blood. These and other relationships between blood types of donors and recipients are summarized in the simple diagram to the right.
Geographic Distribution of ABO Blood Groups
The frequencies of blood groups for the ABO system vary around the world. You can see how the A and B alleles and the blood group O are distributed geographically on the maps in Figure 6.5.6.
- Worldwide, B is the rarest ABO allele, so type B blood is the least common ABO blood type. Only about 16 per cent of all people have the B allele. Its highest frequency is in Asia. Its lowest frequency is among the indigenous people of Australia and the Americas.
- The A allele is somewhat more common around the world than the B allele, so type A blood is also more common than type B blood. The highest frequencies of the A allele are in Australian Aborigines, the Lapps (Sami) of Northern Scandinavia, and Blackfoot Native Americans in North America. The allele is nearly absent among Native Americans in Central and South America.
- The O allele is the most common ABO allele around the world, and type O blood is the most common ABO blood type. Almost two-thirds of people have at least one copy of the O allele. It is especially common in Native Americans in Central and South America, where it reaches frequencies close to 100 per cent. It also has relatively high frequencies in Australian Aborigines and Western Europeans. Its frequencies are lowest in Eastern Europe and Central Asia.
Figure 6.5.6 Maps of populations that have the A, B and O alleles.
Evolution of the ABO Blood Group System
The geographic distribution of ABO blood type alleles provides indirect evidence for the evolutionary history of these alleles. Evolutionary biologists hypothesize that the allele for blood type A evolved first, followed by the allele for blood type O, and then by the allele for blood type B. This chronology accounts for the percentages of people worldwide with each blood group, and is also consistent with known patterns of early population movements.
The evolutionary forces of founder effect and genetic drift have no doubt played a significant role in the current distribution of ABO blood types worldwide. Geographic variation in ABO blood groups is also likely to be influenced by natural selection, because different blood types are thought to vary in their susceptibility to certain diseases. For example:
- People with type O blood may be more susceptible to cholera and plague. They are also more likely to develop gastrointestinal ulcers.
- People with type A blood may be more susceptible to smallpox and more likely to develop certain cancers.
- People with types A, B, and AB blood appear to be less likely to form blood clots that can cause strokes. However, early in our history, the ability of blood to form clots — which appears greater in people with type O blood — may have been a survival advantage.
- Perhaps the greatest natural selective force associated with ABO blood types is malaria. There is considerable evidence to suggest that people with type O blood are somewhat resistant to malaria, giving them a selective advantage where malaria is endemic.
Rhesus Blood Group System
Another well-known blood group system is the Rhesus (Rh) blood group system. The Rhesus system has dozens of different antigens, but only five main antigens (called D, C, c, E, and e). The major Rhesus antigen is the D antigen. People with the D antigen are called Rh positive (Rh+), and people who lack the D antigen are called Rh negative (Rh-). Rhesus antigens are thought to play a role in transporting ions across cell membranes by acting as channel proteins.
The Rhesus blood group system is controlled by two linked genes on chromosome 1. One gene, called RHD, produces a single antigen, antigen D. The other gene, called RHCE, produces the other four relatively common Rhesus antigens (C, c, E, and e), depending on which alleles for this gene are inherited.
Rhesus Blood Group and Transfusions
After the ABO system, the Rhesus system is the second most important blood group system in blood transfusions. The D antigen is the one most likely to provoke an immune response in people who lack the antigen. People who have the D antigen (Rh+) can be safely transfused with either Rh+ or Rh- blood, whereas people who lack the D antigen (Rh-) can be safely transfused only with Rh- blood.
Unlike anti-A and anti-B antibodies to ABO antigens, anti-D antibodies for the Rhesus system are not usually produced by sensitization to environmental substances. People who lack the D antigen (Rh-), however, may produce anti-D antibodies if exposed to Rh+ blood. This may happen accidentally in a blood transfusion, although this is extremely unlikely today. It may also happen during pregnancy with an Rh+ fetus if some of the fetal blood cells pass into the mother’s blood circulation.
Hemolytic Disease of the Newborn
If a woman who is Rh- is carrying an Rh+ fetus, the fetus may be at risk. This is especially likely if the mother has formed anti-D antibodies during a prior pregnancy because of a mixing of maternal and fetal blood during childbirth. Unlike antibodies against ABO antigens, antibodies against the Rhesus D antigen can cross the placenta and enter the blood of the fetus. This may cause hemolytic disease of the newborn (HDN), also called erythroblastosis fetalis, an illness in which fetal red blood cells are destroyed by maternal antibodies, causing anemia. This illness may range from mild to severe. If it is severe, it may cause brain damage and is sometimes fatal for the fetus or newborn. Fortunately, HDN can be prevented by preventing the formation of anti-D antibodies in the Rh- mother. This is achieved by injecting the mother with a medication called Rho(D) immune globulin.
Geographic Distribution of Rhesus Blood Types
The majority of people worldwide are Rh+, but there is regional variation in this blood group system, as there is with the ABO system. The aboriginal inhabitants of the Americas and Australia originally had very close to 100 per cent Rh+ blood. The frequency of the Rh+ blood type is also very high in African populations, at about 97 to 99 per cent. In East Asia, the frequency of Rh+ is slightly lower, at about 93 to 99 per cent. Europeans have the lowest frequency of the Rh+ blood type at about 83 to 85 per cent.
What explains the population variation in Rhesus blood types? Prior to the advent of modern medicine, Rh+ positive children conceived by Rh- women were at risk of fetal or newborn death or impairment from HDN. This was an enigma, because presumably, natural selection would work to remove the rarer phenotype (Rh-) from populations. However, the frequency of this phenotype is relatively high in many populations.
Recent studies have found evidence that natural selection may actually favor heterozygotes for the Rhesus D antigen. The selective agent in this case is thought to be toxoplasmosis, a parasitic disease caused by the protozoan Toxoplasma gondii, which is very common worldwide. You can see a life cycle diagram of the parasite in Figure 6.5.7. Infection by this parasite often causes no symptoms at all, or it may cause flu-like symptoms for a few days or weeks. Exposure to the parasite has been linked, however, to increased risk of mental disorders (such as schizophrenia), neurological disorders (such as Alzheimer’s), and other neurological problems, including delayed reaction times. One study found that people who tested positive for antibodies to the parasite were more than twice as likely to be involved in traffic accidents.
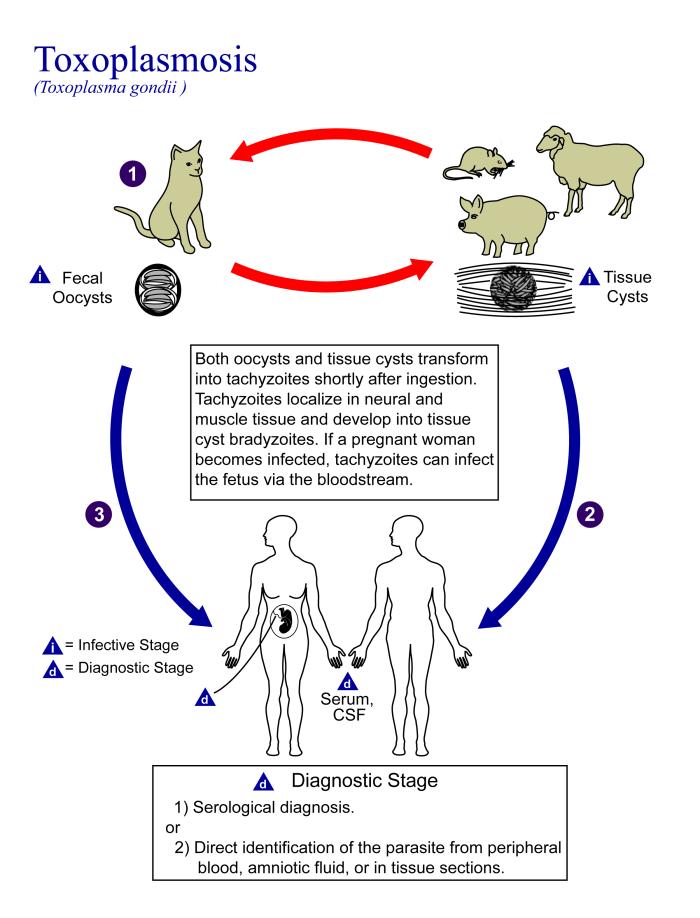
People who are heterozygous for the D antigen appear less likely to develop the negative neurological and mental effects of Toxoplasma gondii infection. This could help explain why both phenotypes (Rh+ and Rh-) are maintained in most populations. There are also striking geographic differences in the prevalence of toxoplasmosis worldwide, ranging from zero to 95 per cent in different regions. This could explain geographic variation in the D antigen worldwide, because its strength as a selective agent would vary with its prevalence.
Feature: Myth vs. Reality
Myth |
Reality |
| “Your nutritional needs can be determined by your ABO blood type. Knowing your blood type allows you to choose the appropriate foods that will help you lose weight, increase your energy, and live a longer, healthier life.” | This idea was proposed in 1996 in a New York Times bestseller Eat Right for Your Type, by Peter D’Adamo, a naturopath. Naturopathy is a method of treating disorders that involves the use of herbs, sunlight, fresh air, and other natural substances. Some medical doctors consider naturopathy a pseudoscience. A major scientific review of the blood type diet could find no evidence to support it. In one study, adults eating the diet designed for blood type A showed improved health — but this occurred in everyone, regardless of their blood type. Because the blood type diet is based solely on blood type, it fails to account for other factors that might require dietary adjustments or restrictions. For example, people with diabetes — but different blood types — would follow different diets, and one or both of the diets might conflict with standard diabetes dietary recommendations and be dangerous. |
| “ABO blood type is associated with certain personality traits. People with blood type A, for example, are patient and responsible, but may also be stubborn and tense, whereas people with blood type B are energetic and creative, but may also be irresponsible and unforgiving. In selecting a spouse, both your own and your potential mate’s blood type should be taken into account to ensure compatibility of your personalities.” | The belief that blood type is correlated with personality is widely held in Japan and other East Asian countries. The idea was originally introduced in the 1920s in a study commissioned by the Japanese government, but it was later shown to have no scientific support. The idea was revived in the 1970s by a Japanese broadcaster, who wrote popular books about it. There is no scientific basis for the idea, and it is generally dismissed as pseudoscience by the scientific community. Nonetheless, it remains popular in East Asian countries, just as astrology is popular in many other countries. |
6.5 Summary
- Blood type (or blood group) is a genetic characteristic associated with the presence or absence of antigens on the surface of red blood cells. A blood group system refers to all of the gene(s), alleles, and possible genotypes and phenotypes that exist for a particular set of blood type antigens.
- Antigens are molecules that the immune system identifies as either self or non-self. If antigens are identified as non-self, the immune system responds by forming antibodies that are specific to the non-self antigens, leading to the destruction of cells bearing the antigens.
- The ABO blood group system is a system of red blood cell antigens controlled by a single gene with three common alleles on chromosome 9. There are four possible ABO blood types: A, B, AB, and O. The ABO system is the most important blood group system in blood transfusions. People with type O blood are universal donors, and people with type AB blood are universal recipients.
- The frequencies of ABO blood type alleles and blood groups vary around the world. The allele for the B antigen is least common, and blood type O is the most common. The evolutionary forces of founder effect, genetic drift, and natural selection are responsible for the geographic distribution of ABO alleles and blood types. People with type O blood, for example, may be somewhat resistant to malaria, possibly giving them a selective advantage where malaria is endemic.
- The Rhesus blood group system is a system of red blood cell antigens controlled by two genes with many alleles on chromosome 1. There are five common Rhesus antigens, of which antigen D is most significant. Individuals who have antigen D are called Rh+, and individuals who lack antigen D are called Rh-. Rh- mothers of Rh+ fetuses may produce antibodies against the D antigen in the fetal blood, causing hemolytic disease of the newborn (HDN).
- The majority of people worldwide are Rh+, but there is regional variation in this blood group system. This variation may be explained by natural selection that favors heterozygotes for the D antigen, because this genotype seems to be protected against some of the neurological consequences of the common parasitic infection toxoplasmosis.
6.5 Review Questions
- Define blood type and blood group system.
- Explain the relationship between antigens and antibodies.
- Identify the alleles, genotypes, and phenotypes in the ABO blood group system.
- Discuss the medical significance of the ABO blood group system.
- Compare the relative worldwide frequencies of the three ABO alleles.
- Give examples of how different ABO blood types vary in their susceptibility to diseases.
- Describe the Rhesus blood group system.
- Relate Rhesus blood groups to blood transfusions.
- What causes hemolytic disease of the newborn?
- Describe how toxoplasmosis may explain the persistence of the Rh- blood type in human populations.
- A woman is blood type O and Rh-, and her husband is blood type AB and Rh+. Answer the following questions about this couple and their offspring.
- What are the possible genotypes of their offspring in terms of ABO blood group?
- What are the possible phenotypes of their offspring in terms of ABO blood group?
- Can the woman donate blood to her husband? Explain your answer.
- Can the man donate blood to his wife? Explain your answer.
- Type O blood is characterized by the presence of O antigens — explain why this statement is false.
- Explain why newborn hemolytic disease may be more likely to occur in a second pregnancy than in a first.
6.5 Explore More
Why do blood types matter? – Natalie S. Hodge, TED-Ed, 2015.
How do blood transfusions work? – Bill Schutt, TED-Ed, 2020.
Attributes
Figure 6.5.1
Following the Blood Donation Trail by EJ Hersom/ USA Department of Defense is in the public domain. [Disclaimer: The appearance of U.S. Department of Defense (DoD) visual information does not imply or constitute DoD endorsement.]
Figure 6.5.2
Antibody by Fvasconcellos on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.5.3
ABO system codominance.svg, adapted by YassineMrabet (original “Codominant” image from US National Library of Medicine) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.5.4
ABO_blood_type.svg by InvictaHOG on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 6.5.5
Blood Donor and recipient ABO by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
Figure 6.5.6
- Map of Blood Group A by Muntuwandi at en.wikipedia on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/) license.
- Map of Blood Group B by Muntuwandi at en.wikipedia on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/) license.
- Map of Blood Group O by anthro palomar at en.wikipedia on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/) license.
Figure 6.5.7
Toxoplasma_gondii_Life_cycle_PHIL_3421_lores by Alexander J. da Silva, PhD/Melanie Moser, Centers for Disease Control and Prevention‘s Public Health Image Library (PHIL#3421) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Table 6.5.1
ABO Blood Group System: Genotypes and Phenotypes was created by Christine Miller.
References
Dean, L. (2005). Chapter 4 Hemolytic disease of the newborn. In Blood Groups and Red Cell Antigens [Internet]. National Center for Biotechnology Information (US). https://www.ncbi.nlm.nih.gov/books/NBK2266/
Mayo Clinic Staff. (n.d.). Toxoplasmosis [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/toxoplasmosis/symptoms-causes/syc-20356249
MedlinePlus. (2019, January 29). Hemolytic transfusion reaction [online article]. U.S. National Library of Medicine. https://en.wikipedia.org/w/index.php?title=Chromosome_9&oldid=946440619
TED-Ed. (2015, June 29). Why do blood types matter? – Natalie S. Hodge. YouTube. https://www.youtube.com/watch?v=xfZhb6lmxjk&feature=youtu.be
TED-Ed. (2020, February 18). How do blood transfusions work? – Bill Schutt. YouTube. https://www.youtube.com/watch?v=qcZKbjYyOfE&feature=youtu.be
Wikipedia contributors. (2020, May 10). Chromosome 1. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Chromosome_1&oldid=955942444
Wikipedia contributors. (2020, March 20). Chromosome 9. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Chromosome_9&oldid=946440619
A body fluid in humans and other animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells. In vertebrates, it is composed of blood cells suspended in blood plasma.
A classification of blood, based on the presence and absence of antibodies and inherited antigenic substances on the surface of red blood cells.
A sequence of nucleotides in DNA or RNA that codes for a molecule that has a function.
A variant form of a given gene, meaning it is one of two or more versions of a known mutation at the same place on a chromosome. It can also refer to different sequence variations for a several-hundred base-pair or more region of the genome that codes for a protein.
The part of the genetic makeup of a cell, and therefore of any individual, which determines one of its characteristics (phenotype).
The set of observable characteristics of an individual resulting from the interaction of its genotype with the environment.
Molecules on the surface of cells or viruses that the immune system identifies as either self (produced by your own body) or non-self (not produced by your own body).
The part of each hemisphere of the cerebrum that is involved in functions such as touch, reading, and arithmetic.
A biomolecule consisting of carbon (C), hydrogen (H) and oxygen (O) atoms, usually with a hydrogen–oxygen atom ratio of 2:1. Complex carbohydrates are polymers made from monomers of simple carbohydrates, also termed monosaccharides.
An antibody, also known as an immunoglobulin, is a large, Y-shaped protein produced mainly by plasma cells that is used by the immune system to neutralize pathogens such as pathogenic bacteria and viruses.
The loss of genetic variation that occurs when a new population is established by a very small number of individuals from a larger population.
Variation in the relative frequency of different genotypes in a small population, owing to the chance disappearance of particular genes as individuals die or do not reproduce.
The differential survival and reproduction of individuals due to differences in phenotype. It is a key mechanism of evolution, the change in the heritable traits characteristic of a population over generations.
A condition in which you don't have enough healthy red blood cells to carry adequate oxygen to the body's tissues resulting in symptoms including weakness and fatigue.
A disease that results from infection with the Toxoplasma gondii parasite, one of the world's most common parasites. Infection usually occurs by eating undercooked contaminated meat, exposure from infected cat feces, or mother-to-child transmission during pregnancy.


