125 14.3 Heart
Created by CK-12 Foundation/Adapted by Christine Miller

Lub, Dub
Lub dub, lub dub, lub dub… That’s how the sound of a beating heart is typically described. Those are also the only two sounds that should be audible when listening to a normal, healthy heart through a stethoscope, as in Figure 14.3.1. If a doctor hears something different from the normal lub dub sounds, it’s a sign of a possible heart abnormality. What causes the heart to produce the characteristic lub dub sounds? Read on to find out.
Introduction to the Heart
The heart is a muscular organ behind the sternum (breastbone), slightly to the left of the center of the chest. A normal adult heart is about the size of a fist. The function of the heart is to pump blood through blood vessels of the cardiovascular system. The continuous flow of blood through the system is necessary to provide all the cells of the body with oxygen and nutrients, and to remove their metabolic wastes.
Structure of the Heart
The heart has a thick muscular wall that consists of several layers of tissue. Internally, the heart is divided into four chambers through which blood flows. Because of heart valves, blood flows in just one direction through the chambers.
Heart Wall
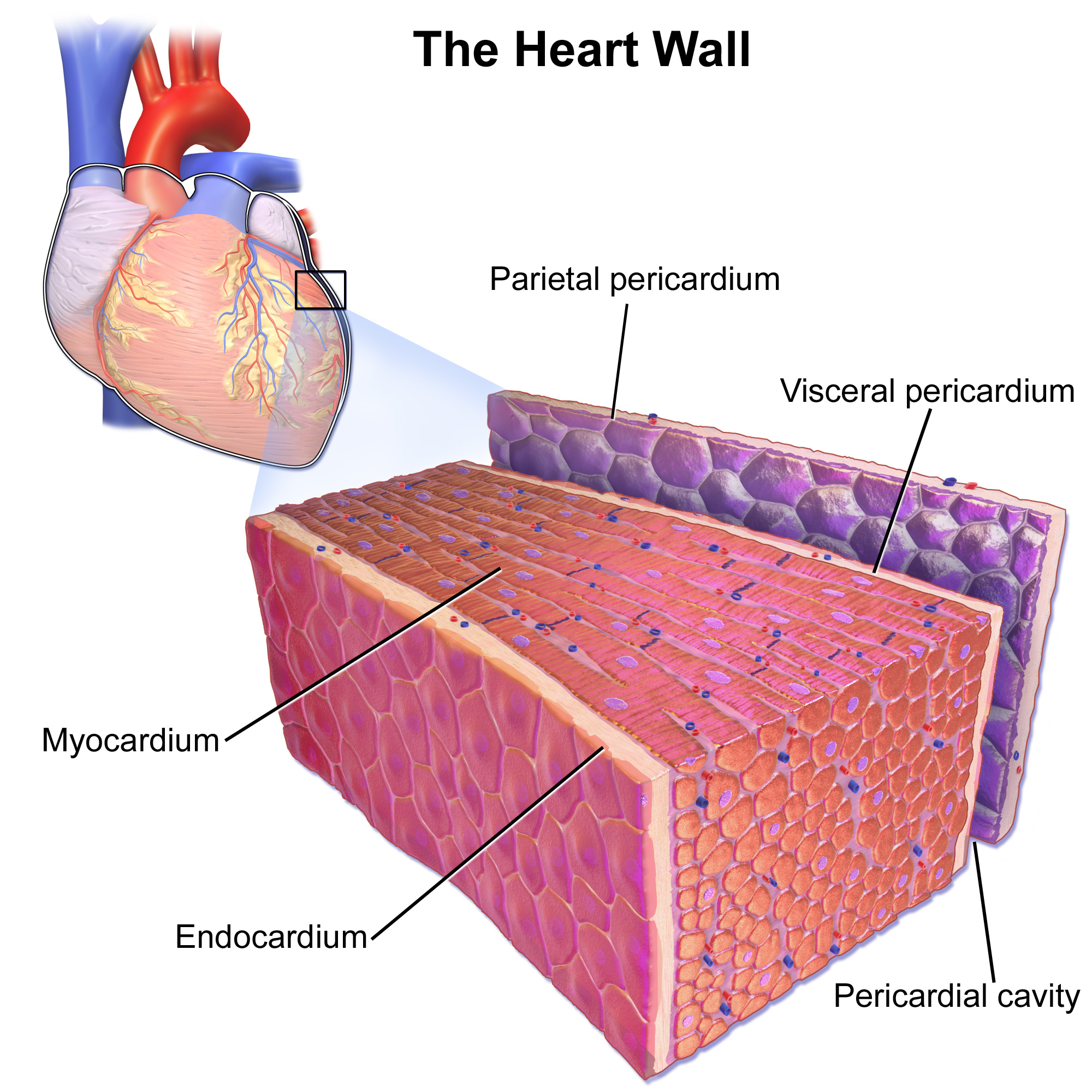
As shown in Figure 14.3.2, the wall of the heart is made up of three layers, called the endocardium, myocardium, and pericardium.
- The endocardium is the innermost layer of the heart wall. It is made up primarily of simple epithelial cells. It covers the heart chambers and valves. A thin layer of connective tissue joins the endocardium to the myocardium.
- The myocardium is the middle and thickest layer of the heart wall. It consists of cardiac muscle surrounded by a framework of collagen. There are two types of cardiac muscle cells in the myocardium: cardiomyocytes — which have the ability to contract easily — and pacemaker cells, which conduct electrical impulses that cause the cardiomyocytes to contract. About 99 per cent of cardiac muscle cells are cardiomyocytes, and the remaining one per cent is pacemaker cells. The myocardium is supplied with blood vessels and nerve fibres via the pericardium.
- The pericardium is a protective sac that encloses and protects the heart. The pericardium consists of two membranes (visceral pericardium and parietal pericardium), between which there is a fluid-filled cavity. The fluid helps to cushion the heart, and also lubricates its outer surface.
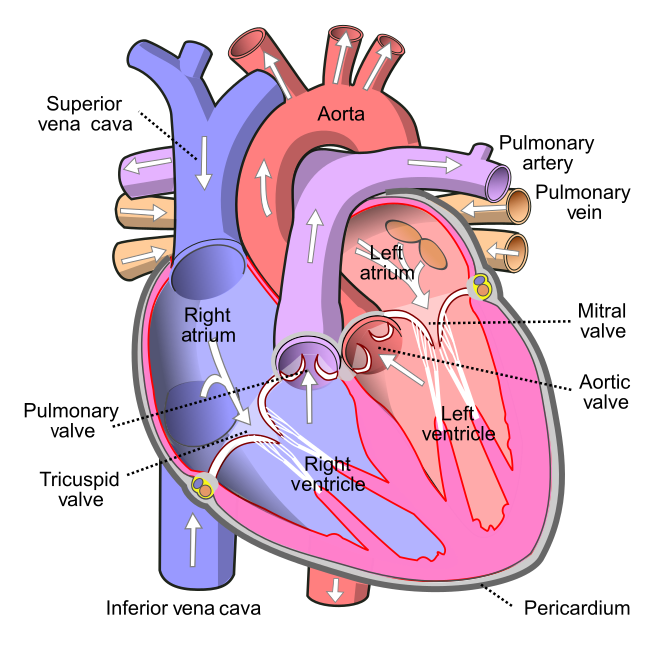
Heart Chambers
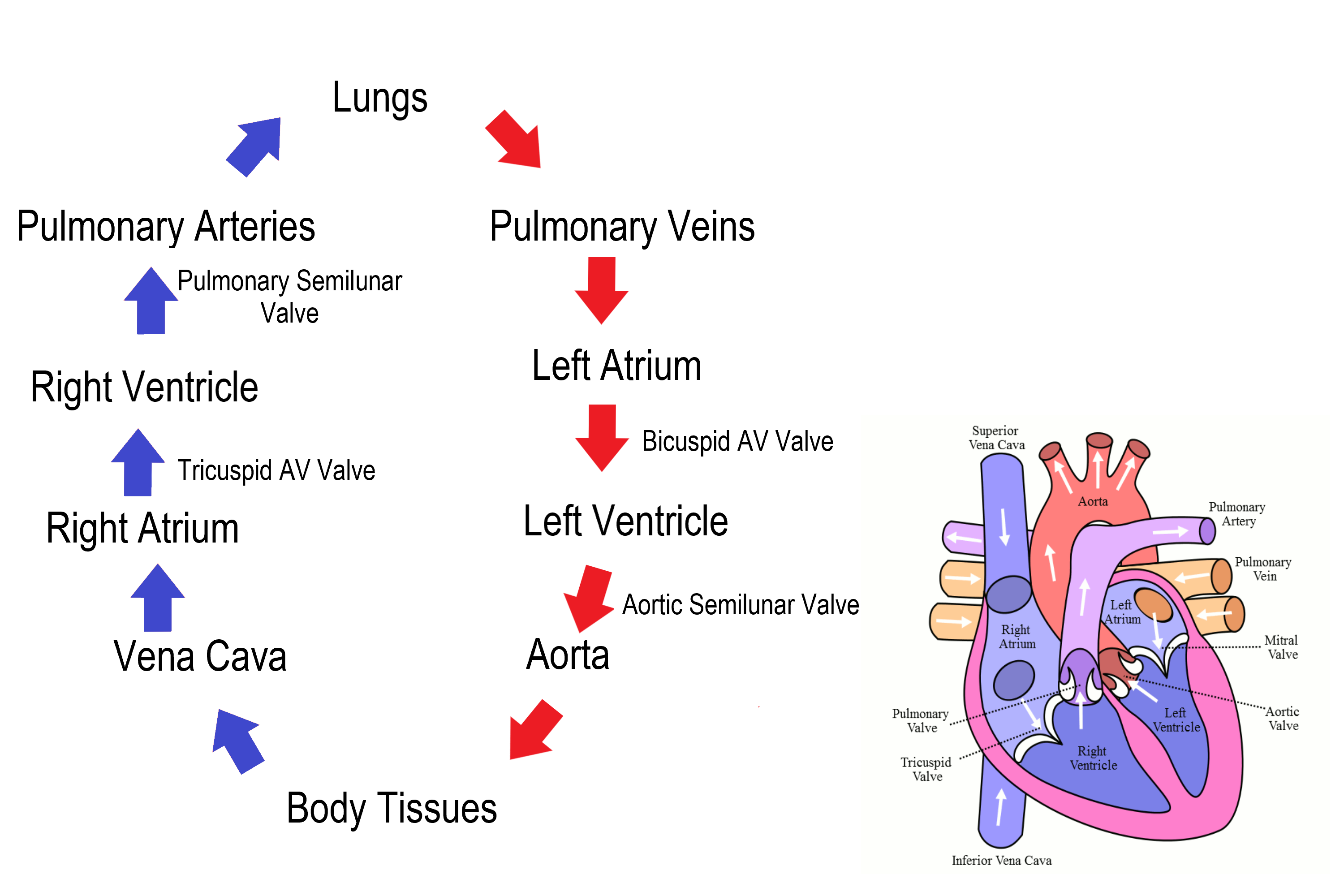
As shown in Figure 14.3.3 the four chambers of the heart include two upper chambers called atria (singular, atrium), and two lower chambers called ventricles. The atria are also referred to as receiving chambers, because blood coming into the heart first enters these two chambers. The right atrium receives deoxygenated blood from the upper and lower body through the superior vena cava and inferior vena cava, respectively. The left atrium receives oxygenated blood from the lungs through the pulmonary veins. The ventricles are also referred to as discharging chambers, because blood leaving the heart passes out through these two chambers. The right ventricle discharges blood to the lungs through the pulmonary artery, and the left ventricle discharges blood to the rest of the body through the aorta. The four chambers are separated from each other by dense connective tissue consisting mainly of collagen.
Heart Valves
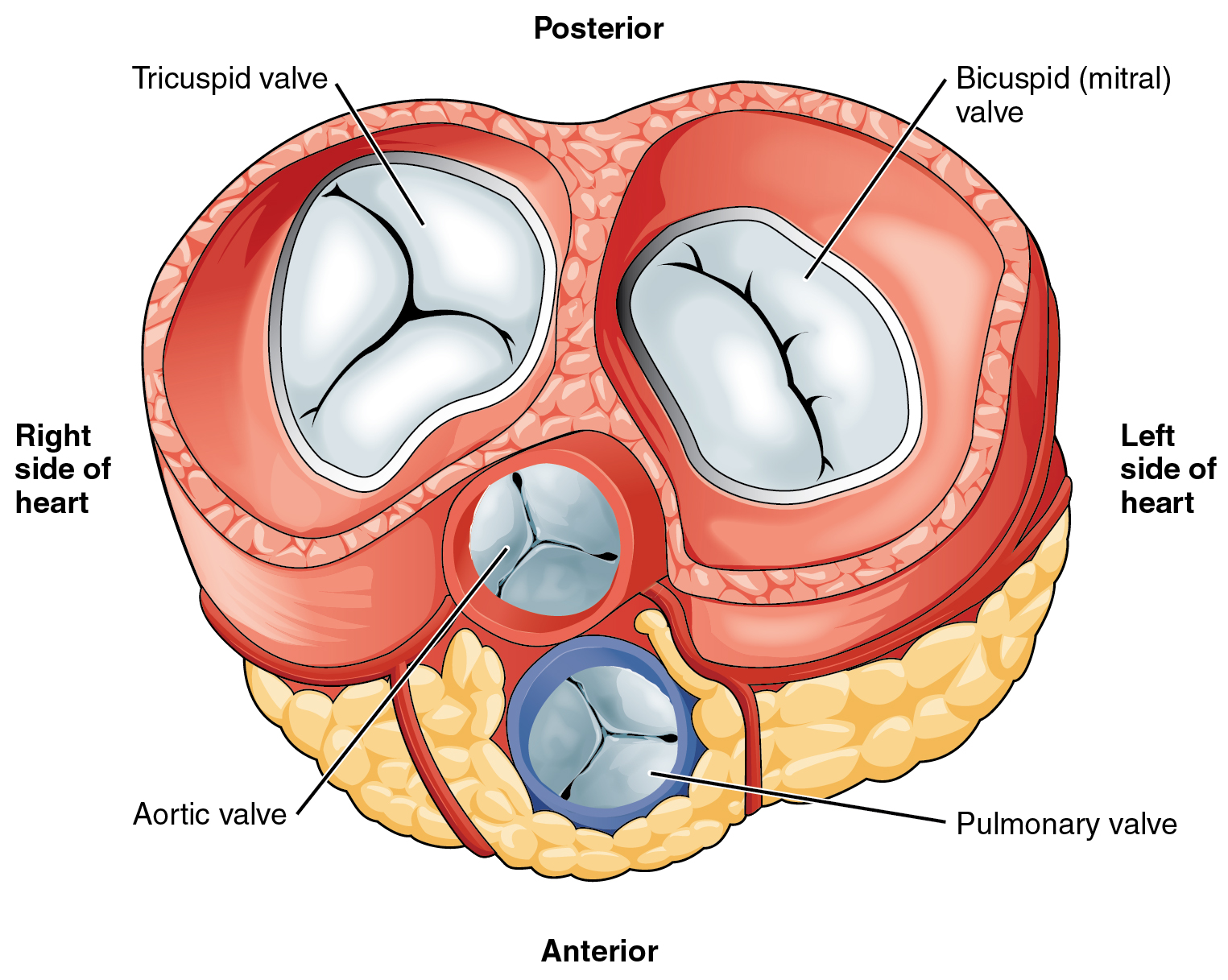
Figure 14.3.4 shows the location of the heart’s four valves in a top-down view, looking down at the heart as if the arteries and veins feeding into and out of the heart were removed. The heart valves allow blood to flow from the atria to the ventricles, and from the ventricles to the pulmonary artery and aorta. The valves are constructed in such a way that blood can flow through them in only one direction, thus preventing the backflow of blood. Figure 14.3.5 shows how valves open to let blood into the appropriate chamber, and then close to prevent blood from moving in the wrong direction and the next chamber contracts. The four valves are the:
- Tricuspid atrioventricular valve, (can be shortened to tricuspid AV valve) which allows blood to flow from the right atrium to the right ventricle.
- Bicuspid atrioventricular valve (also know as the mitral valve), which allows blood to flow from the left atrium to the left ventricle.
- Pulmonary semilunar valve, which allows blood to flow from the right ventricle to the pulmonary artery.
- Aortic semilunar valve, which allows blood to flow from the left ventricle to the aorta.
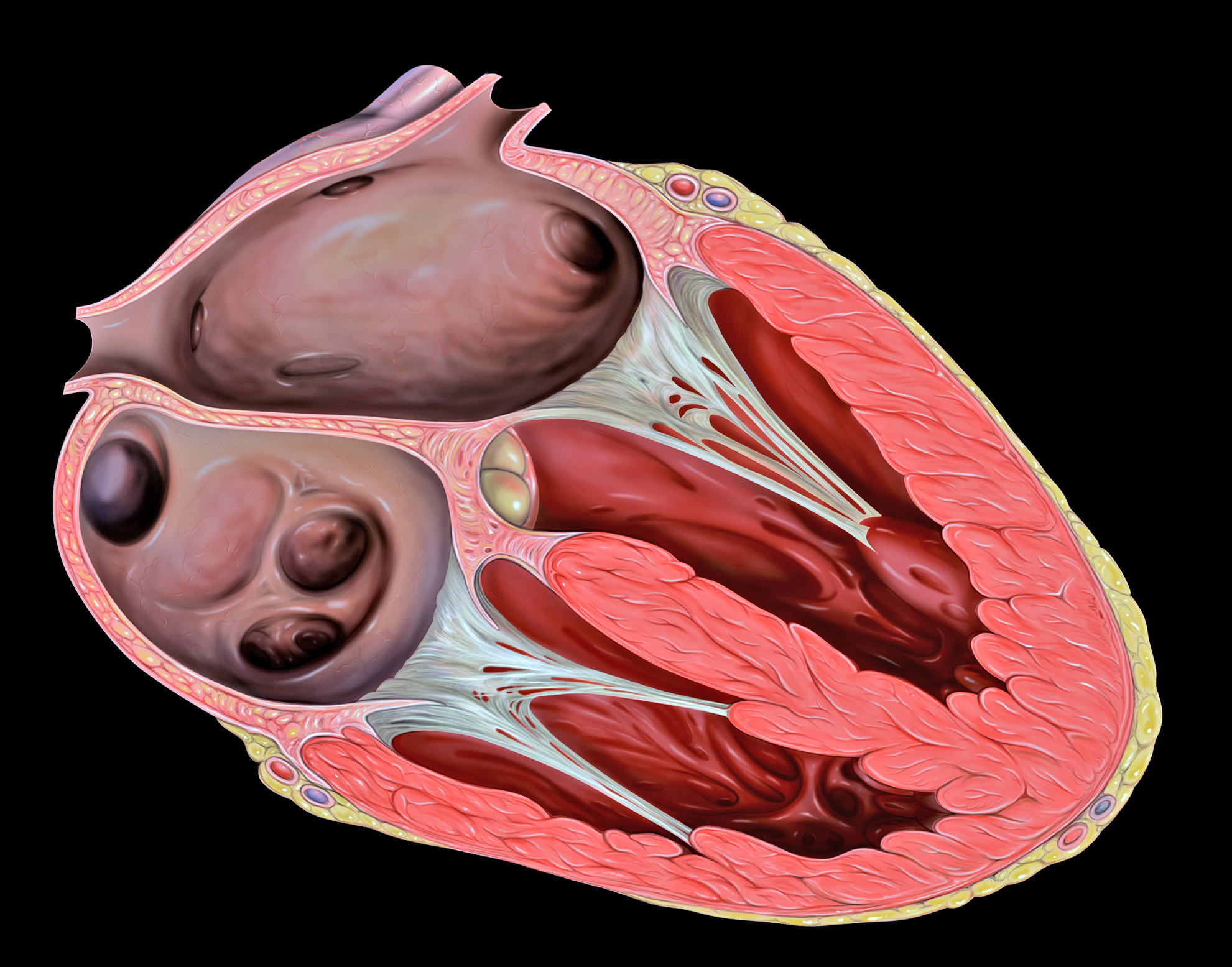
The two atrioventricular (AV) valves prevent backflow when the ventricles are contracting, while the semilunar valves prevent backflow from vessels. This means that the AV valves must withstand much more pressure than do the semilunar valves. In order to withstand the force of the ventricles contracting (to prevent blood from backflowing into the atria), the AV valves are reinforced with structures called chordae tendineae — tendon-like cords of connective tissue which anchor the valve and prevent it from prolapse. Figure 14.3.6 shows the structure and location of the chordae tendoneae.
The chordae tendoneae are under such force that they need special attachments to the interior of the ventricles where they anchor. Papillary muscles are specialized muscles in the interior of the ventricle that provide a strong anchor point for the chordae tendineae.
Coronary Circulation
The cardiomyocytes of the muscular walls of the heart are very active cells, because they are responsible for the constant beating of the heart. These cells need a continuous supply of oxygen and nutrients. The carbon dioxide and waste products they produce also must be continuously removed. The blood vessels that carry blood to and from the heart muscle cells make up the coronary circulation. Note that the blood vessels of the coronary circulation supply heart tissues with blood, and are different from the blood vessels that carry blood to and from the chambers of the heart as part of the general circulation. Coronary arteries supply oxygen-rich blood to the heart muscle cells. Coronary veins remove deoxygenated blood from the heart muscles cells.
- There are two coronary arteries — a right coronary artery that supplies the right side of the heart, and a left coronary artery that supplies the left side of the heart. These arteries branch repeatedly into smaller and smaller arteries and finally into capillaries, which exchange gases, nutrients, and waste products with cardiomyocytes.
- At the back of the heart, small cardiac veins drain into larger veins, and finally into the great cardiac vein, which empties into the right atrium. At the front of the heart, small cardiac veins drain directly into the right atrium.
Blood Circulation Through the Heart
Figure 14.3.7 shows how blood circulates through the chambers of the heart. The right atrium collects blood from two large veins, the superior vena cava (from the upper body) and the inferior vena cava (from the lower body). The blood that collects in the right atrium is pumped through the tricuspid valve into the right ventricle. From the right ventricle, the blood is pumped through the pulmonary valve into the pulmonary artery. The pulmonary artery carries the blood to the lungs, where it enters the pulmonary circulation, gives up carbon dioxide, and picks up oxygen. The oxygenated blood travels back from the lungs through the pulmonary veins (of which there are four), and enters the left atrium of the heart. From the left atrium, the blood is pumped through the mitral valve into the left ventricle. From the left ventricle, the blood is pumped through the aortic valve into the aorta, which subsequently branches into smaller arteries that carry the blood throughout the rest of the body. After passing through capillaries and exchanging substances with cells, the blood returns to the right atrium via the superior vena cava and inferior vena cava, and the process begins anew.
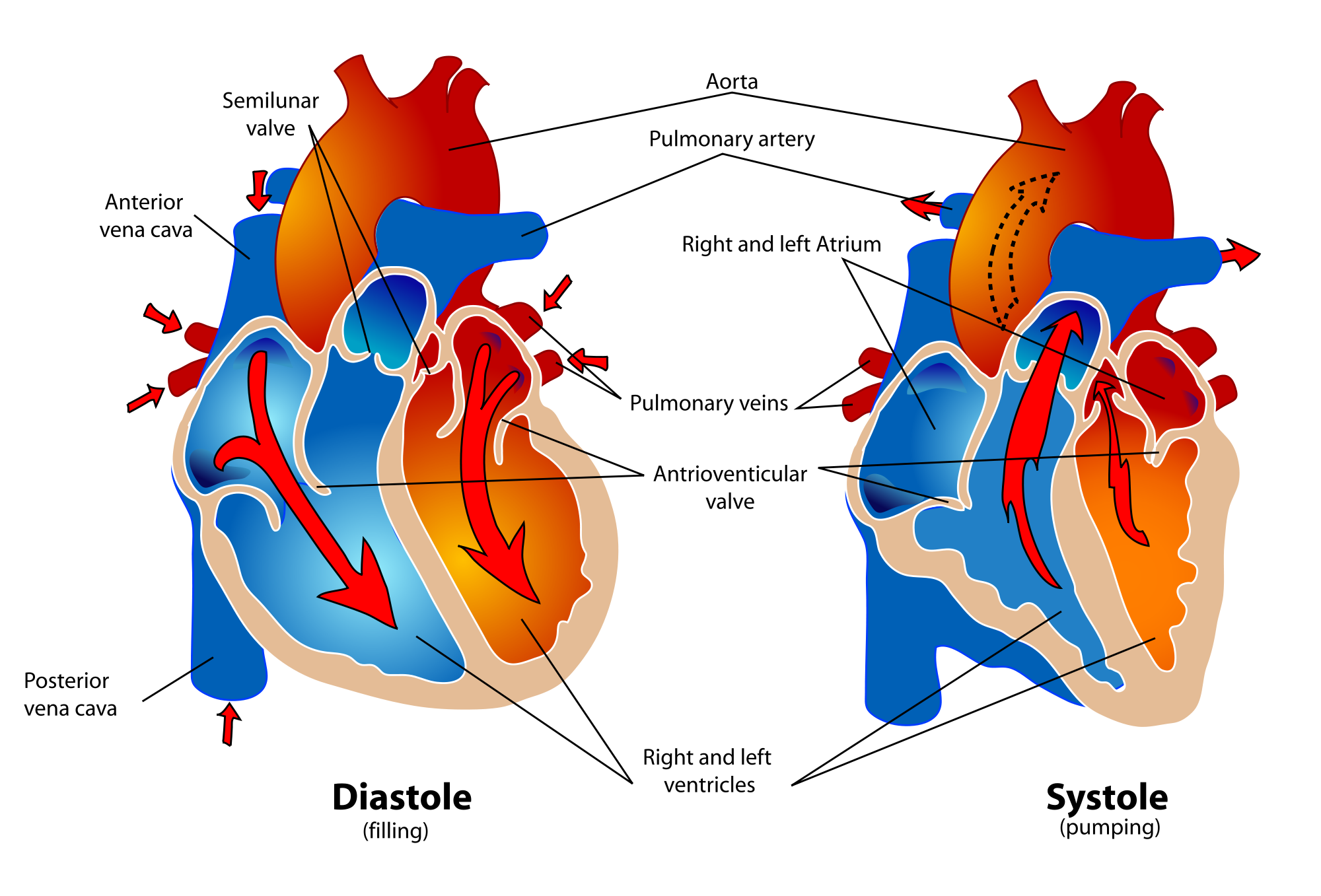
Cardiac Cycle
The cardiac cycle refers to a single complete heartbeat, which includes one iteration of the lub and dub sounds heard through a stethoscope. During the cardiac cycle, the atria and ventricles work in a coordinated fashion so that blood is pumped efficiently through and out of the heart. The cardiac cycle includes two parts, called diastole and systole, which are illustrated in the diagrams in Figure 14.3.8.
- During diastole, the atria contract and pump blood into the ventricles, while the ventricles relax and fill with blood from the atria.
- During systole, the atria relax and collect blood from the lungs and body, while the ventricles contract and pump blood out of the heart.
Electrical Stimulation of the Heart
The normal, rhythmical beating of the heart is called sinus rhythm. It is established by the heart’s pacemaker cells, which are located in an area of the heart called the sinoatrial node (shown in Figure 14.3.9). The pacemaker cells create electrical signals with the movement of electrolytes (sodium, potassium, and calcium ions) into and out of the cells. For each cardiac cycle, an electrical signal rapidly travels first from the sinoatrial node, to the right and left atria so they contract together. Then, the signal travels to another node, called the atrioventricular node (Figure 14.3.9), and from there to the right and left ventricles (which also contract together), just a split second after the atria contract.
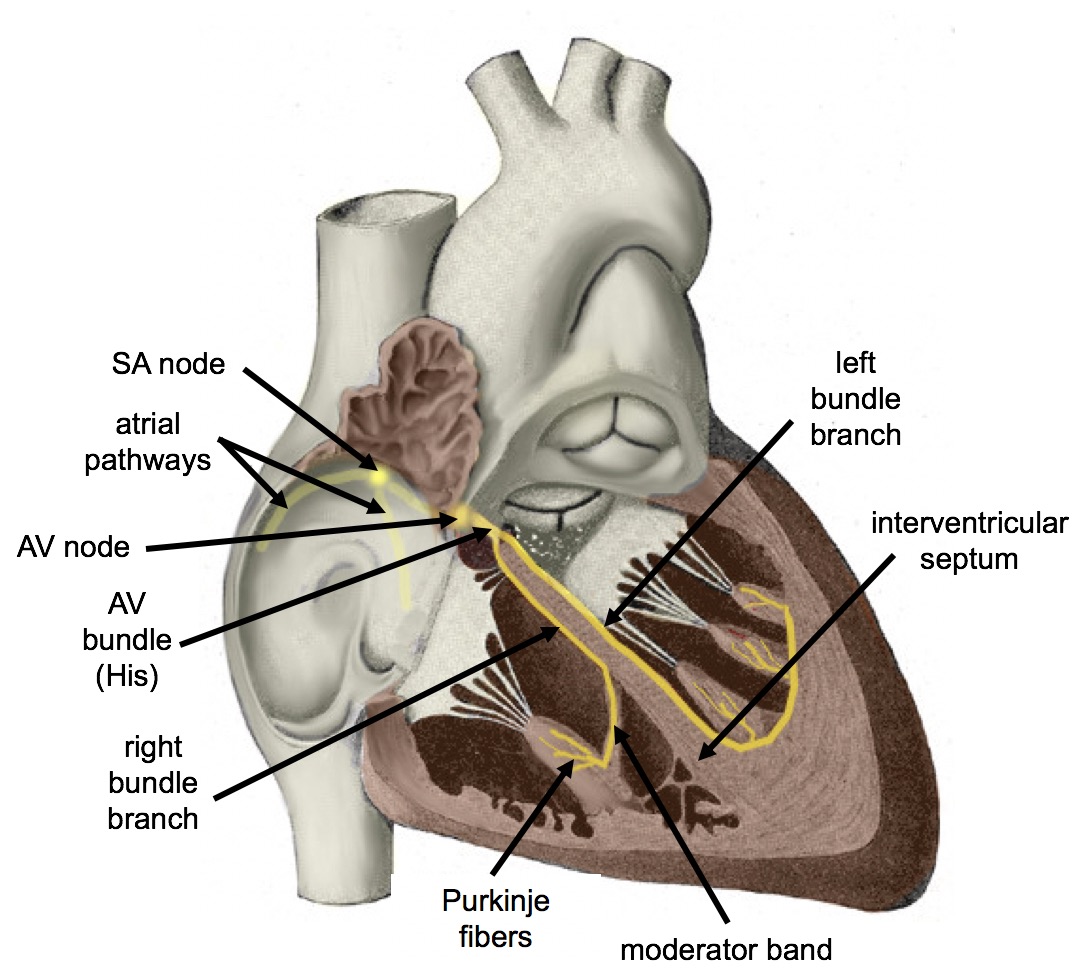
The normal sinus rhythm of the heart is influenced by the autonomic nervous system through sympathetic and parasympathetic nerves. These nerves arise from two paired cardiovascular centers in the medulla of the brainstem. The parasympathetic nerves act to decrease the heart rate, and the sympathetic nerves act to increase the heart rate. Parasympathetic input normally predominates. Without it, the pacemaker cells of the heart would generate a resting heart rate of about 100 beats per minute, instead of a normal resting heart rate of about 72 beats per minute. The cardiovascular centers receive input from receptors throughout the body, and act through the sympathetic nerves to increase the heart rate, as needed. Increased physical activity, for example, is detected by receptors in muscles, joints, and tendons. These receptors send nerve impulses to the cardiovascular centers, causing sympathetic nerves to increase the heart rate, and allowing more blood to flow to the muscles.
Besides the autonomic nervous system, other factors can also affect the heart rate. For example, thyroid hormones and adrenal hormones (such as epinephrine) can stimulate the heart to beat faster. The heart rate also increases when blood pressure drops or the body is dehydrated or overheated. On the other hand, cooling of the body and relaxation — among other factors — can contribute to a decrease in the heart rate.
Feature: Human Biology in the News
When a patient’s heart is too diseased or damaged to sustain life, a heart transplant is likely to be the only long-term solution. The first successful heart transplant was undertaken in South Africa in 1967. There are over 2,200 Canadians walking around today because of life-saving heart transplant surgery. Approximately 180 heart transplant surgeries are performed each year, but there are still so many Canadians on the transplant list that some die while waiting for a heart. The problem is that far too few hearts are available for transplant — there is more demand (people waiting for a heart transplant) than supply (organ donors). Sometimes, recipient hopefuls will receive a device called a Total Artificial Heart (see Figure 14.3.10), which can buy them some time until a donor heart becomes available.
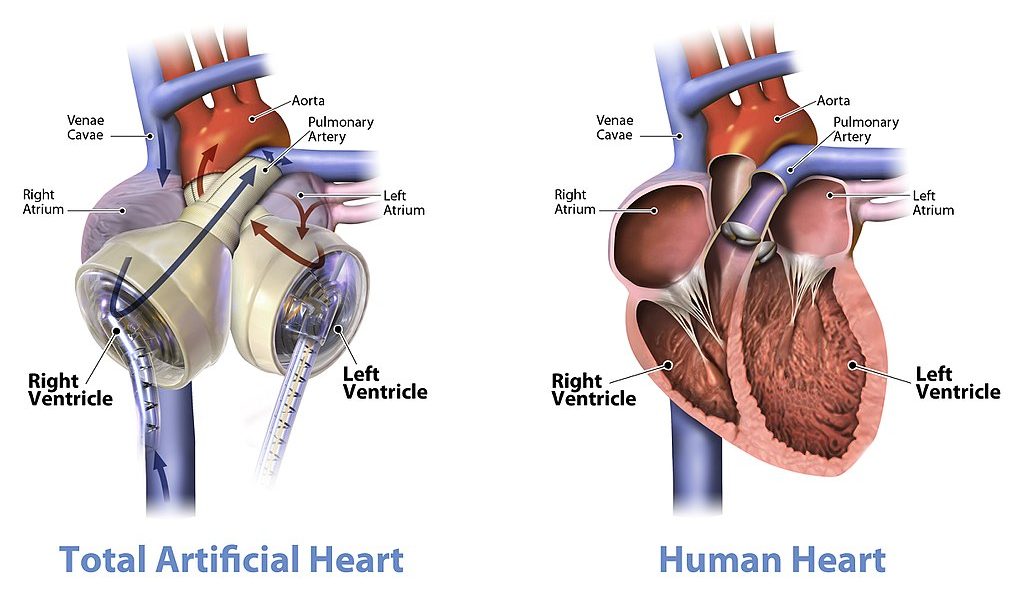
Watch the video below “Total artificial heart option…” from Stanford Health Care to see how it works:
Total artificial heart option at Stanford (Includes surgical graphic footage), Stanford Health Care, 2014.
14.3 Summary
- The heart is a muscular organ behind the sternum and slightly to the left of the center of the chest. Its function is to pump blood through the blood vessels of the cardiovascular system.
- The wall of the heart consists of three layers. The middle layer, the myocardium, is the thickest layer and consists mainly of cardiac muscle. The interior of the heart consists of four chambers, with an upper atrium and lower ventricle on each side of the heart. Blood enters the heart through the atria, which pump it to the ventricles. Then the ventricles pump blood out of the heart. Four valves in the heart keep blood flowing in the correct direction and prevent backflow.
- The coronary circulation consists of blood vessels that carry blood to and from the heart muscle cells, and is different from the general circulation of blood through the heart chambers. There are two coronary arteries that supply the two sides of the heart with oxygenated blood. Cardiac veins drain deoxygenated blood back into the heart.
- Deoxygenated blood flows into the right atrium through veins from the upper and lower body (superior and inferior vena cava, respectively), and oxygenated blood flows into the left atrium through four pulmonary veins from the lungs. Each atrium pumps the blood to the ventricle below it. From the right ventricle, deoxygenated blood is pumped to the lungs through the two pulmonary arteries. From the left ventricle, oxygenated blood is pumped to the rest of the body through the aorta.
- The cardiac cycle refers to a single complete heartbeat. It includes diastole — when the atria contract — and systole, when the ventricles contract.
- The normal, rhythmic beating of the heart is called sinus rhythm. It is established by the heart’s pacemaker cells in the sinoatrial node. Electrical signals from the pacemaker cells travel to the atria, and cause them to contract. Then, the signals travel to the atrioventricular node and from there to the ventricles, causing them to contract. Electrical stimulation from the autonomic nervous system and hormones from the endocrine system can also influence heartbeat.
14.3 Review Questions
- What is the heart, where is located, and what is its function?
-
- Describe the coronary circulation.
- Summarize how blood flows into, through, and out of the heart.
- Explain what controls the beating of the heart.
- What are the two types of cardiac muscle cells in the myocardium? What are the differences between these two types of cells?
- Explain why the blood from the cardiac veins empties into the right atrium of the heart. Focus on function (rather than anatomy) in your answer.
14.3 Explore More
Noel Bairey Merz: The single biggest health threat women face, TED, 2012.
Watch a Transcatheter Aortic Valve Replacement (TAVR) Procedure at St. Luke’s in Cedar Rapids, Iowa, UnityPoint Health – Cedar Rapids, 2018.
A Change of Heart: My Transplant Experience | Thomas Volk | TEDxUWLaCrosse, TEDx Talks, 2018.
Heart Transplant Recipient Meets Donor Family For The First Time, WMC Health, 2018.
Attributions
Figure 14.3.1
- Female clinician dressed in scrubs using a stethoscope by Amanda Mills, USCDCP, on Pixnio is used under a CC0 public domain certification license (https://creativecommons.org/licenses/publicdomain/).
- Human heart beating loud and strong (audio) by Daniel Simion on Soundbible.com is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.3.2
Blausen_0470_HeartWall by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.3.3
Diagram_of_the_human_heart_(cropped).svg by Wapcaplet on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license.
Figure 14.3.4
Heart_Valves by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 14.3.5
CG_Heart Valve Animation by DrJanaOfficial on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 14.3.6
Heart_tee_four_chamber_view by Patrick J. Lynch, medical illustrator from Yale University School of Medicine, on Wikimedia Commons is used under a CC BY 2.5 (https://creativecommons.org/licenses/by/2.5) license.
Figure 14.3.7
Circulation of blood through the heart by Christinelmiller on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license. [Original image in the bottom right is by Wapcaplet / CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0/)]
Figure 14.3.8
Human_healthy_pumping_heart_en.svg by Mariana Ruiz Villarreal [LadyofHats] on Wikimedia Common is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 14.3.9
Cardiac_Conduction_System by Cypressvine on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 19.12 Heart valves with the atria and major vessels removed [digital image]. In Anatomy and Physiology (Section 19.1). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/19-1-heart-anatomy#fig-ch20_01_04
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Heart and Stroke Foundation of Canada. (n.d.). https://www.heartandstroke.ca/
Sliwa, K., Zilla, P. (2017, December 7). 50th anniversary of the first human heart transplant—How is it seen today? European Heart Journal, 38(46):3402–3404. https://doi.org/10.1093/eurheartj/ehx695
Stanford Health Care. (2014, December 3). Total artificial heart option at Stanford (Includes surgical graphic footage). YouTube. https://www.youtube.com/watch?v=1PtxaxcPnGc&feature=youtu.be
TED. (2012, March 21). Noel Bairey Merz: The single biggest health threat women face. YouTube. https://www.youtube.com/watch?v=1bnzVjOJ6NM&feature=youtu.be
TEDx Talks. (2018, April 18). A change of heart: My transplant experience | Thomas Volk | TEDxUWLaCrosse. YouTube. https://www.youtube.com/watch?v=zU6mmix04PI&feature=youtu.be
UMagazine. (2015, Fall). The cutting edge: Patient first to bridge from experimental total artificial heart to transplant. UCLA Health. https://www.uclahealth.org/u-magazine/patient-first-to-bridge-from-experimental-total-artificial-heart-to-transplant
UnityPoint Health – Cedar Rapids. (2018, February 7). Watch a transcatheter aortic valve replacement (TAVR) Procedure at St. Luke’s in Cedar Rapids, Iowa. YouTube. https://www.youtube.com/watch?v=jJm7zBcN6-M&feature=youtu.be
WMC Health. (2018, September 13). Heart transplant recipient meets donor family for the first time. YouTube. https://www.youtube.com/watch?v=biGuwQhuAsk&feature=youtu.be
A muscular organ in the chest that pumps blood through blood vessels when it contracts.
Refers to the body system consisting of the heart, blood vessels and the blood. Blood contains oxygen and other nutrients which your body needs to survive. The body takes these essential nutrients from the blood.
A body fluid in humans and other animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells. In vertebrates, it is composed of blood cells suspended in blood plasma.
The thin, smooth membrane which lines the inside of the chambers of the heart and forms the surface of the valves.
The muscular tissue of the heart.
Involuntary, striated muscle found only in the walls of the heart; also called myocardium.
The membrane enclosing the heart, consisting of an outer fibrous layer and an inner double layer of serous membrane.
One of the two upper chambers of the heart that pumps blood to the ventricle below it. Plural form is atria.
One of two lower chambers of the heart that pumps blood out of the heart.
A large vein carrying deoxygenated blood into the heart. There are two in humans, the inferior vena cava (carrying blood from the lower body) and the superior vena cava (carrying blood from the head, arms, and upper body).
A vein carrying oxygenated blood from the lungs to the left atrium of the heart.
The artery carrying blood from the right ventricle of the heart to the lungs for oxygenation.
The main artery of the body, supplying oxygenated blood to the circulatory system. In humans it passes over the heart from the left ventricle and runs down in front of the backbone.
The main structural protein in the extracellular matrix in the various connective tissues in the body. As the main component of connective tissue, it is the most abundant protein in mammals, making up from 25% to 35% of the whole-body protein content.
A valve in the heart which forms the boundary between the right ventricle and the right atrium. Deoxygenated blood enters the right side of the heart via the inferior and superior vena cava. It contains three flap-like cusps that, when closed, keep blood from regressing back into the right atrium.
A valve which permits blood to flow one way only, from the left atrium into the left ventricle This valve is more commonly called the mitral valve because it has two flaps (cusps) and looks like a bishop's miter or headdress.
The semilunar valve of the heart that lies between the right ventricle and the pulmonary artery and has three cusps (sometimes referred to as the pulmonic valve).
A semilunar valve in the hearth that separates the left ventricle and the aorta; preventing backflow of blood.
Tendon-resembling fibrous cords of connective tissue (sometimes referred to as the heart strings) that connect the papillary muscles to the tricuspid AV valve and the bicuspid AV valve in the heart.
In medicine, prolapse is a condition in which organs fall down or slip out of place. It is used for organs protruding through the vagina, rectum, or for the misalignment of the valves of the heart.
One of the small bundles of muscles attached to the ventricle walls and to the chordae tendineae that tighten these tendons during ventricular contraction.
A cardiac muscle cell. The cell is striated, containing thick and thin proteins arranged linearly. These filaments are composed, like other striated muscle cells, largely of actin and myosin. The cell has an abundant supply of mitochondria that supply the energy needed by the cell for regular muscular contraction.
Part of the systemic circulatory system that supplies blood to and provides drainage from the tissues of the heart.
One of two arteries that supply the cells of the heart with oxygen and nutrients.
A part of a heartbeat (cardiac cycle) in which the atria contract and pump blood into the ventricles, while the ventricles relax and fill with blood from the atria.
The part of a heartbeat in which the atria relax and fill with blood from the lungs and body, while the ventricles contract and pump blood out of the heart.
The normal, rhythmical beating of the heart.
A type of cells located in the heart that create electrical signals to stimulate heart muscles to contract.
A small body of specialized muscle tissue in the wall of the right atrium of the heart that acts as a pacemaker by producing a contractile signal at regular intervals.
The performance of the human heart from the ending of one heartbeat to the beginning of the next. It consists of two periods: one during which the heart muscle relaxes and refills with blood, called diastole, following a period of robust contraction and pumping of blood, dubbed systole.
A part of the electrical conduction system of the heart that coordinates the top of the heart. It electrically connects the atria and ventricles.
A division of the peripheral nervous system that controls involuntary activities.
A long stem-like structure which makes up part of the brainstem. It is anterior and partially inferior to the cerebellum. It is responsible for autonomic (involuntary) functions ranging from vomiting to sneezing.
A large endocrine gland in the neck whose hormones control the rate of cellular metabolism and help maintain calcium homeostasis.
one of a pair of glands located on top of the kidneys that secretes hormones such as cortisol and adrenaline
The body system which acts as a chemical messenger system comprising feedback loops of the hormones released by internal glands of an organism directly into the circulatory system, regulating distant target organs. In humans, the major endocrine glands are the thyroid gland and the adrenal glands.

