136 15.7 Disorders of the Gastrointestinal Tract
Created by CK-12 Foundation/Adapted by Christine Miller

Crohn’s Rash
If you had a skin rash like the one shown in Figure 15.7.1, you probably wouldn’t assume that it was caused by a digestive system disease. However, that’s exactly why the individual in the picture has a rash. He has a gastrointestinal (GI) tract disorder called Crohn’s disease. This disease is one of a group of GI tract disorders that are known collectively as inflammatory bowel disease. Unlike other inflammatory bowel diseases, signs and symptoms of Crohn’s disease may not be confined to the GI tract.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is a collection of inflammatory conditions primarily affecting the intestines. The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Unlike Crohn’s disease — which may affect any part of the GI tract and the joints, as well as the skin — ulcerative colitis mainly affects just the colon and rectum. Both diseases occur when the body’s own immune system attacks the digestive system. Both diseases typically first appear in the late teens or early twenties, and occur equally in males and females. Approximately 270,000 Canadians are currently living with IBD, 7,000 of which are children. The annual cost of caring for these Canadians is estimated at $1.28 billion. The number of cases of IBD has been steadily increasing and it is expected that by 2030 the number of Canadians suffering from IBD will grow to 400,000.
Crohn’s Disease
Crohn’s disease is a type of inflammatory bowel disease that may affect any part of the GI tract from the mouth to the anus, among other body tissues. The most commonly affected region is the ileum, which is the final part of the small intestine. Signs and symptoms of Crohn’s disease typically include abdominal pain, diarrhea (with or without blood), fever, and weight loss. Malnutrition because of faulty absorption of nutrients may also occur. Potential complications of Crohn’s disease include obstructions and abscesses of the bowel. People with Crohn’s disease are also at slightly greater risk than the general population of developing bowel cancer. Although there is a slight reduction in life expectancy in people with Crohn’s disease, if the disease is well-managed, affected people can live full and productive lives. Approximately 135,000 Canadians are living with Crohn’s disease.
Crohn’s disease is caused by a combination of genetic and environmental factors that lead to impairment of the generalized immune response (called innate immunity). The chronic inflammation of Crohn’s disease is thought to be the result of the immune system “trying” to compensate for the impairment. Dozens of genes are likely to be involved, only a few of which have been identified. Because of the genetic component, close relatives such as siblings of people with Crohn’s disease are many times more likely to develop the disease than people in the general population. Environmental factors that appear to increase the risk of the disease include smoking tobacco and eating a diet high in animal proteins. Crohn’s disease is typically diagnosed on the basis of a colonoscopy, which provides a direct visual examination of the inside of the colon and the ileum of the small intestine.
People with Crohn’s disease typically experience recurring periods of flare-ups followed by remission. There are no medications or surgical procedures that can cure Crohn’s disease, although medications such as anti-inflammatory or immune-suppressing drugs may alleviate symptoms during flare-ups and help maintain remission. Lifestyle changes, such as dietary modifications and smoking cessation, may also help control symptoms and reduce the likelihood of flare-ups. Surgery may be needed to resolve bowel obstructions, abscesses, or other complications of the disease.
Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease that causes inflammation and ulcers (sores) in the colon and rectum. Unlike Crohn’s disease, other parts of the GI tract are rarely affected in ulcerative colitis. The primary symptoms of the disease are lower abdominal pain and bloody diarrhea. Weight loss, fever, and anemia may also be present. Symptoms typically occur intermittently with periods of no symptoms between flare-ups. People with ulcerative colitis have a considerably increased risk of colon cancer and should be screened for colon cancer more frequently than the general population. Ulcerative colitis, however, seems to primarily reduce the quality of life, and not the lifespan.
The exact cause of ulcerative colitis is not known. Theories about its cause involve immune system dysfunction, genetics, changes in normal gut bacteria, and lifestyle factors, such as a diet high in animal protein and the consumption of alcoholic beverages. Genetic involvement is suspected in part because ulcerative colitis tens to “run” in families. It is likely that multiple genes are involved. Diagnosis is typically made on the basis of colonoscopy and tissue biopsies.
Lifestyle changes, such as reducing the consumption of animal protein and alcohol, may improve symptoms of ulcerative colitis. A number of medications are also available to treat symptoms and help prolong remission. These include anti-inflammatory drugs and drugs that suppress the immune system. In cases of severe disease, removal of the colon and rectum may be required and can cure the disease.
Diverticulitis
Diverticulitis is a digestive disease in which tiny pouches in the wall of the large intestine become infected and inflamed. Symptoms typically include lower abdominal pain of sudden onset. There may also be fever, nausea, diarrhea or constipation, and blood in the stool. Having large intestine pouches called diverticula (see Figure 15.7.2) that are not inflamed is called diverticulosis. Diverticulosis is thought to be caused by a combination of genetic and environmental factors, and is more common in people who are obese. Infection and inflammation of the pouches (diverticulitis) occurs in about 10–25% of people with diverticulosis, and is more common at older ages. The infection is generally caused by bacteria.
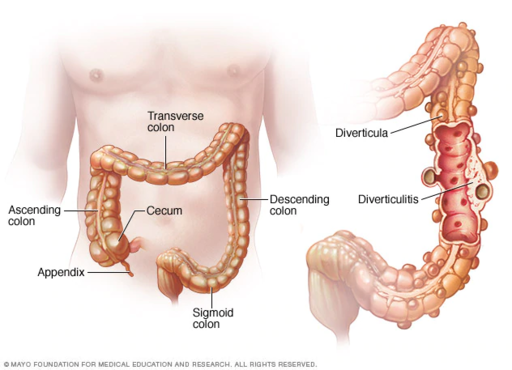
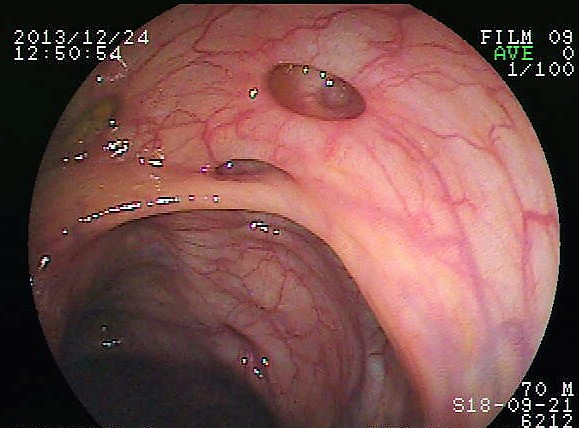
Diverticulitis can usually be diagnosed with a CT scan and can be monitored with a colonoscopy (as seen in Figure 15.7.3). Mild diverticulitis may be treated with oral antibiotics and a short-term liquid diet. For severe cases, intravenous antibiotics, hospitalization, and complete bowel rest (no nourishment via the mouth) may be recommended. Complications such as abscess formation or perforation of the colon require surgery.
Peptic Ulcer
A peptic ulcer is a sore in the lining of the stomach or the duodenum (first part of the small intestine). If the ulcer occurs in the stomach, it is called a gastric ulcer. If it occurs in the duodenum, it is called a duodenal ulcer. The most common symptoms of peptic ulcers are upper abdominal pain that often occurs in the night and improves with eating. Other symptoms may include belching, vomiting, weight loss, and poor appetite. Many people with peptic ulcers, particularly older people, have no symptoms. Peptic ulcers are relatively common, with about ten per cent of people developing a peptic ulcer at some point in their life.
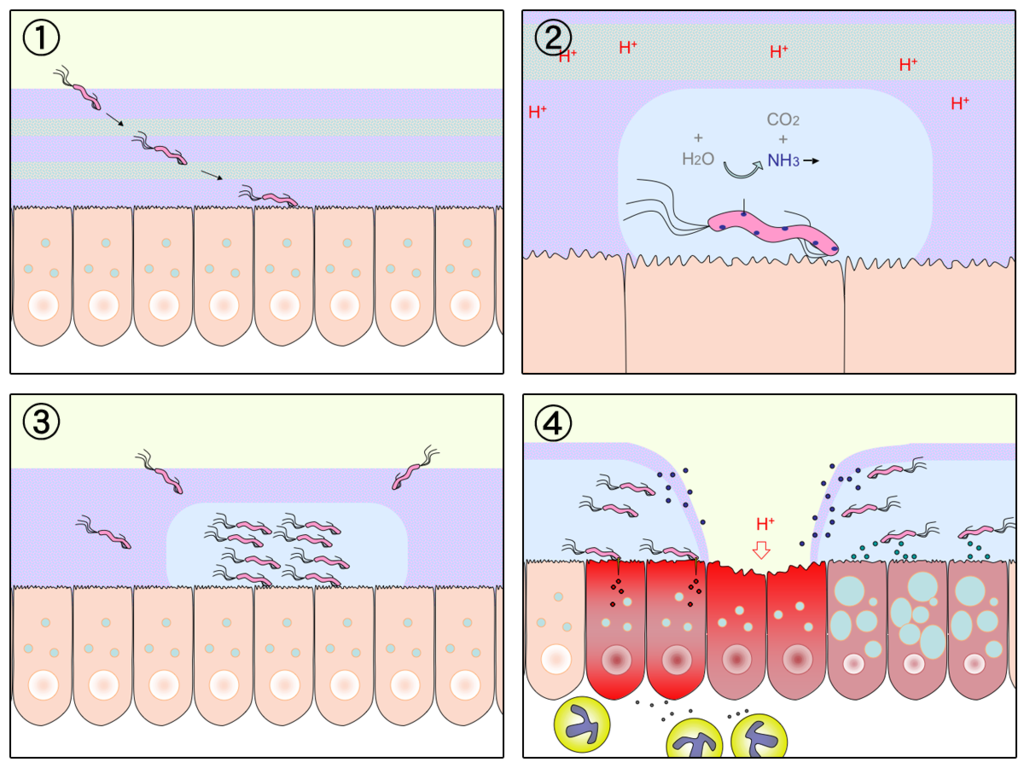
The most common cause of peptic ulcers is infection with the bacterium Helicobacter pylori, which may be transmitted by food, contaminated water, or human saliva (for example, by kissing or sharing eating utensils). Surprisingly, the bacterial cause of peptic ulcers was not discovered until the 1980s. The scientists who made the discovery are Australians Robin Warren and Barry J. Marshall. Although the two scientists eventually won a Nobel Prize for their discovery, their hypothesis was poorly received at first. To demonstrate the validity of their discovery, Marshall used himself in an experiment. He drank a culture of bacteria from a peptic ulcer patient and developed symptoms of peptic ulcer in a matter of days. His symptoms resolved on their own within a couple of weeks, but, at his wife’s urging, he took antibiotics to kill any remaining bacteria. Marshall’s self-experiment was published in the Australian Medical Journal, and is among the most cited articles ever published in the journal. Figure 15.7.4 shows how H. pylori cause peptic ulcers.
Another relatively common cause of peptic ulcers is chronic use of non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen. Additional contributing factors may include tobacco smoking and stress, although these factors have not been demonstrated conclusively to cause peptic ulcers independent of H. pylori infection. Contrary to popular belief, diet does not appear to play a role in either causing or preventing peptic ulcers. Eating spicy foods and drinking coffee and alcohol were once thought to cause peptic ulcers. These lifestyle choices are no longer thought to have much (if any) of an effect on the development of peptic ulcers.
Peptic ulcers are typically diagnosed on the basis of symptoms or the presence of H. pylori in the GI tract. However, endoscopy (shown in Figure 15.7.5), which allows direct visualization of the stomach and duodenum with a camera, may be required for a definitive diagnosis. Peptic ulcers are usually treated with antibiotics to kill H. pylori, along with medications to temporarily decrease stomach acid and aid in healing. Unfortunately, H. pylori has developed resistance to commonly used antibiotics, so treatment is not always effective. If a peptic ulcer has penetrated so deep into the tissues that it causes a perforation of the wall of the stomach or duodenum, then emergency surgery is needed to repair the damage.

Gastroenteritis
Gastroenteritis, also known as infectious diarrhea or stomach flu, is an acute and usually self-limiting infection of the GI tract by pathogens. Symptoms typically include some combination of diarrhea, vomiting, and abdominal pain. Fever, lack of energy, and dehydration may also occur. The illness generally lasts less than two weeks, even without treatment, but in young children it is potentially deadly. Gastroenteritis is very common, especially in poorer nations. Worldwide, up to five billion cases occur each year, resulting in about 1.4 million deaths.
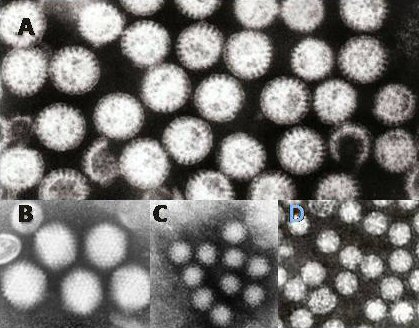
Commonly called “stomach flu,” gastroenteritis is unrelated to the influenza virus, although viruses are the most common cause of the disease (see Figure 15.7.6). In children, rotavirus is most often the cause which is why the British Columbia immunization schedule now includes a rotovirus vaccine. Norovirus is more likely to be the cause of gastroenteritis in adults. Besides viruses, other potential causes of gastroenteritis include fungi, bacteria (most often E. coli or Campylobacter jejuni), and protozoa(including Giardia lamblia, more commonly called Beaver Fever, described below). Transmission of pathogens may occur due to eating improperly prepared foods or foods left to stand at room temperature, drinking contaminated water, or having close contact with an infected individual.
Gastroenteritis is less common in adults than children, partly because adults have acquired immunity after repeated exposure to the most common infectious agents. Adults also tend to have better hygiene than children. If children have frequent repeated incidents of gastroenteritis, they may suffer from malnutrition, stunted growth, and developmental delays. Many cases of gastroenteritis in children can be avoided by giving them a rotavirus vaccine. Frequent and thorough handwashing can cut down on infections caused by other pathogens.
Treatment of gastroenteritis generally involves increasing fluid intake to replace fluids lost in vomiting or diarrhea. Oral rehydration solution, which is a combination of water, salts, and sugar, is often recommended. In severe cases, intravenous fluids may be needed. Antibiotics are not usually prescribed, because they are ineffective against viruses that cause most cases of gastroenteritis.
Giardiasis
Giardiasis, popularly known as beaver fever, is a type of gastroenteritis caused by a GI tract parasite, the single-celled protozoan Giardia lamblia (pictured in Figure 15.7.7). In addition to human beings, the parasite inhabits the digestive tract of a wide variety of domestic and wild animals, including cows, rodents, and sheep, as well as beavers (hence its popular name). Giardiasis is one of the most common parasitic infections in people the world over, with hundreds of millions of people infected worldwide each year.

Transmission of G. lamblia is via a fecal-oral route (as in, you got feces in your food). Those at greatest risk include travelers to countries where giardiasis is common, people who work in child-care settings, backpackers and campers who drink untreated water from lakes or rivers, and people who have close contact with infected people or animals in other settings. In Canada, Giardia is the most commonly identified intestinal parasite and approximately 3,000 Canadians will contract the parasite annually.
Symptoms of giardiasis can vary widely. About one-third third of people with the infection have no symptoms, whereas others have severe diarrhea with poor absorption of nutrients. Problems with absorption occur because the parasites inhibit intestinal digestive enzyme production, cause detrimental changes in microvilli lining the small intestine, and kill off small intestinal epithelial cells. The illness can result in weakness, loss of appetite, stomach cramps, vomiting, and excessive gas. Without treatment, symptoms may continue for several weeks. Treatment with anti-parasitic medications may be needed if symptoms persist longer or are particularly severe.
15.7 Summary
- Inflammatory bowel disease is a collection of inflammatory conditions primarily affecting the intestines. The diseases involve the immune system attacking the GI tract, and they have multiple genetic and environmental causes. Typical symptoms include abdominal pain and diarrhea, which show a pattern of repeated flare-ups interrupted by periods of remission. Lifestyle changes and medications may control flare-ups and extend remission. Surgery is sometimes required.
- The two principal inflammatory bowel diseases are Crohn’s disease and ulcerative colitis. Crohn’s disease may affect any part of the GI tract from the mouth to the anus, among other body tissues. Ulcerative colitis affects the colon and/or rectum.
- Some people have little pouches, called diverticula, in the lining of their large intestine, a condition called diverticulosis. People with diverticulosis may develop diverticulitis, in which one or more of the diverticula become infected and inflamed. Diverticulitis is generally treated with antibiotics and bowel rest. Sometimes, surgery is required.
- A peptic ulcer is a sore in the lining of the stomach (gastric ulcer) or duodenum (duodenal ulcer). The most common cause is infection with the bacterium Helicobacter pylori. NSAIDs (such as aspirin) can also cause peptic ulcers, and some lifestyle factors may play contributing roles. Antibiotics and acid reducers are typically prescribed, and surgery is not often needed.
- Gastroenteritis, or infectious diarrhea, is an acute and usually self-limiting infection of the GI tract by pathogens, most often viruses. Symptoms typically include diarrhea, vomiting, and/or abdominal pain. Treatment includes replacing lost fluids. Antibiotics are not usually effective.
- Giardiasis is a type of gastroenteritis caused by infection of the GI tract with the protozoa parasite Giardia lamblia. It may cause malnutrition. Generally self-limiting, severe or long-lasting cases may require antibiotics.
15.7 Review Questions
-
-
- Compare and contrast Crohn’s disease and ulcerative colitis.
- How are diverticulosis and diverticulitis related?
- Identify the cause of giardiasis. Why may it cause malabsorption?
- Name three disorders of the GI tract that can be caused by bacteria.
- Name one disorder of the GI tract that can be helped by anti-inflammatory medications, and one that can be caused by chronic use of anti-inflammatory medications.
- Describe one reason why it can be dangerous to drink untreated water.
15.7 Explore More
Who’s at risk for colon cancer? – Amit H. Sachdev and Frank G. Gress, TED-Ed, 2018.
The surprising cause of stomach ulcers – Rusha Modi, TED-Ed, 2017.
Attributions
Figure 15.7.1
BADAS_Crohn by Dayavathi Ashok and Patrick Kiely/ Journal of medical case reports on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 15.7.2
512px-Ds00070_an01934_im00887_divert_s_gif.webp by Lfreeman04 on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.7.3
Colon_diverticulum by melvil on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 15.7.4
H_pylori_ulcer_diagram by Y_tambe on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license.
Figure 15.7.5
1024px-Endoscopy_training by Yuya Tamai on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 15.7.6
Gastroenteritis_viruses by Dr. Graham Beards [en:User:Graham Beards] at en.wikipedia on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 15.7.7
Giardia_lamblia_SEM_8698_lores by Janice Haney Carr from CDC/ Public Health Image Library (PHIL) ID# 8698 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
References
Ashok, D., & Kiely, P. (2007). Bowel associated dermatosis – arthritis syndrome: a case report. Journal of medical case reports, 1, 81. https://doi.org/10.1186/1752-1947-1-81
Marshall, B. J., Armstrong, J. A., McGechie, D. B., & Glancy, R. J. (1985). Attempt to fulfil Koch’s postulates for pyloric Campylobacter. The Medical Journal of Australia, 142(8), 436–439.
Marshall, B. J., McGechie, D. B., Rogers, P. A., & Glancy, R. J. (1985). Pyloric campylobacter infection and gastroduodenal disease. The Medical Journal of Australia, 142(8), 439–444.
TED-Ed. (2017, September 28). The surprising cause of stomach ulcers – Rusha Modi. YouTube. https://www.youtube.com/watch?v=V_U6czbDHLE&feature=youtu.be
TED-Ed. (2018, January 4). Who’s at risk for colon cancer? – Amit H. Sachdev and Frank G. Gress. YouTube. https://www.youtube.com/watch?v=H5zin8jKeT0&feature=youtu.be
An inflammatory bowel disease that may affect any part of the gastrointestinal tract from the mouth to the anus.
A type of disease in which the immune system attacks the intestines, causing diarrhea and abdominal pain; for example, Crohn’s disease or ulcerative colitis.
An inflammatory bowel disease that causes ulcers (sores) in the colon and rectum.
The body system in humans and other animals that protects the organism by distinguishing foreign tissue and neutralizing potentially pathogenic organisms or substances.
The third portion of the small intestine, between the jejunum and the cecum.The ileum helps to further digest food coming from the stomach and other parts of the small intestine.
A condition in which feces are discharged from the bowels frequently and in a liquid form.
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.
A condition in which you don't have enough healthy red blood cells to carry adequate oxygen to the body's tissues resulting in symptoms including weakness and fatigue.
A disease in which one or more pouches (diverticula) in the large intestine become infected and inflamed.
A condition in which pouches called diverticula form in the wall of the large intestine.
A sore that develops in the lining of the stomach or duodenum most often caused by infection with the bacterium Helicobacter pylori.
An acute and usually self-limiting infection of the gastrointestinal tract by pathogens; also known as infectious diarrhea.
A microorganism which causes disease.
The involuntary process of ejecting matter from the stomach through the mouth.
Any of a group of RNA viruses, some of which cause acute enteritis (inflammation of the lower digestive tract and possibly diarrhea) in humans.
Any of various single-stranded RNA viruses including the Norwalk virus and closely related viruses which cause gastroenteritis.
A type of gastroenteritis caused by a single-celled protozoan parasite named Giardia lamblia that typically spreads through contaminated food or water via a fecal-oral route.
Non-steroidal anti-inflammatory drugs; ex. ibuprofen.

