95 10.3 Epidermis
Created by CK-12 Foundation/Adapted by Christine Miller

Feel the Burn
The person in Figure 10.3.1 is no doubt feeling the burn — sunburn, that is. Sunburn occurs when the outer layer of the skin is damaged by UV light from the sun or tanning lamps. Some people deliberately allow UV light to burn their skin, because after the redness subsides, they are left with a tan. A tan may look healthy, but it is actually a sign of skin damage. People who experience one or more serious sunburns are significantly more likely to develop skin cancer. Natural pigment molecules in the skin help protect it from UV light damage. These pigment molecules are found in the layer of the skin called the epidermis.
What is the Epidermis?
The epidermis is the outer of the two main layers of the skin. The inner layer is the dermis. It averages about 0.10 mm thick, and is much thinner than the dermis. The epidermis is thinnest on the eyelids (0.05 mm) and thickest on the palms of the hands and soles of the feet (1.50 mm). The epidermis covers almost the entire body surface. It is continuous with — but structurally distinct from — the mucous membranes that line the mouth, anus, urethra, and vagina.
Structure of the Epidermis
There are no blood vessels and very few nerve cells in the epidermis. Without blood to bring epidermal cells oxygen and nutrients, the cells must absorb oxygen directly from the air and obtain nutrients via diffusion of fluids from the dermis below. However, as thin as it is, the epidermis still has a complex structure. It has a variety of cell types and multiple layers.
Cells of the Epidermis
There are several different types of cells in the epidermis. All of the cells are necessary for the important functions of the epidermis.
- The epidermis consists mainly of stacks of keratin-producing epithelial cells called keratinocytes. These cells make up at least 90 per cent of the epidermis. Near the top of the epidermis, these cells are also called squamous cells.
- Another eight per cent of epidermal cells are melanocytes. These cells produce the pigment melanin that protects the dermis from UV light.
- About one per cent of epidermal cells are Langerhans cells. These are immune system cells that detect and fight pathogens entering the skin.
- Less than one per cent of epidermal cells are Merkel cells, which respond to light touch and connect to nerve endings in the dermis.
Layers of the Epidermis
The epidermis in most parts of the body consists of four distinct layers. A fifth layer occurs in the palms of the hands and soles of the feet, where the epidermis is thicker than in the rest of the body. The layers of the epidermis are shown in Figure 10.3.2, and described in the following text.
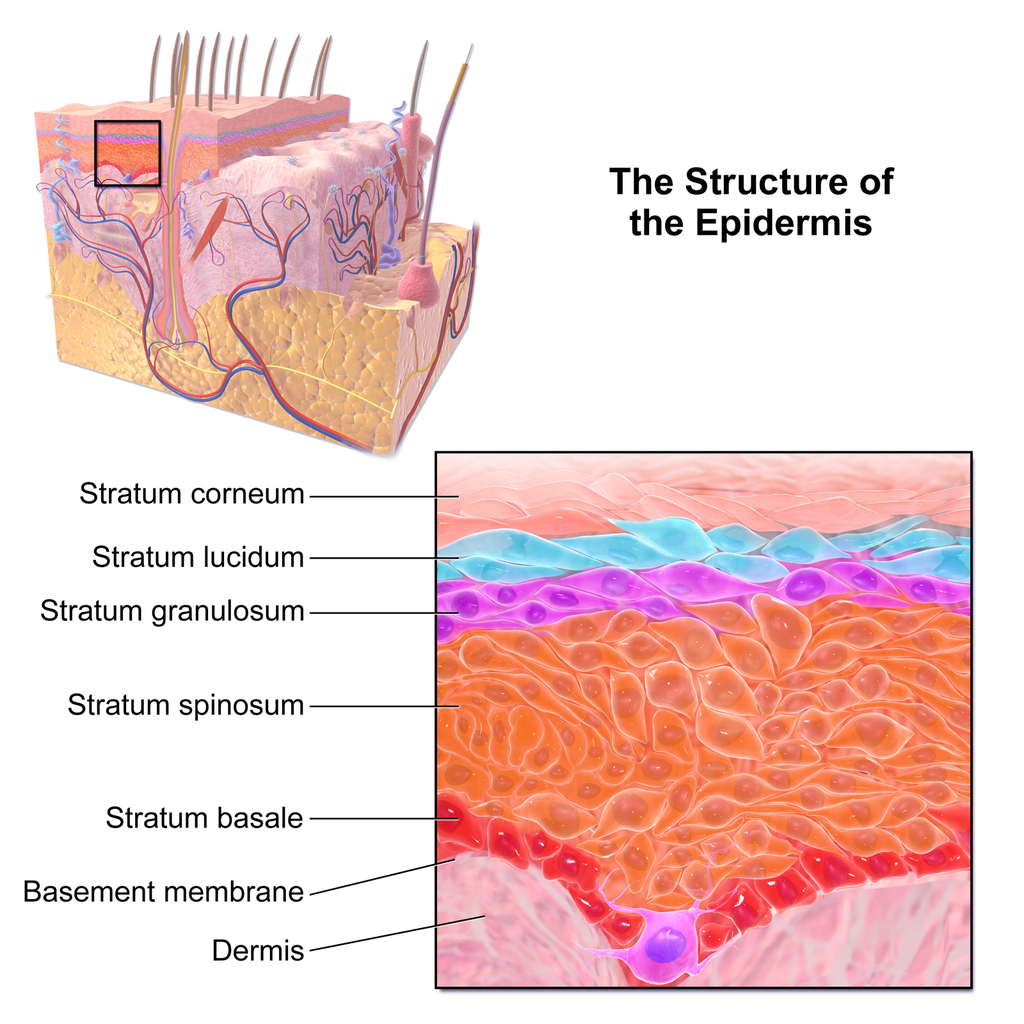
Stratum Basale
The stratum basale is the innermost (or deepest) layer of the epidermis. It is separated from the dermis by a membrane called the basement membrane. The stratum basale contains stem cells — called basal cells — which divide to form all the keratinocytes of the epidermis. When keratinocytes first form, they are cube-shaped and contain almost no keratin. As more keratinocytes are produced, previously formed cells are pushed up through the stratum basale. Melanocytes and Merkel cells are also found in the stratum basale. The Merkel cells are especially numerous in touch-sensitive areas, such as the fingertips and lips.
Stratum Spinosum
Just above the stratum basale is the stratum spinosum. This is the thickest of the four epidermal layers. The keratinocytes in this layer have begun to accumulate keratin, and they have become tougher and flatter. Spiny cellular projections form between the keratinocytes and hold them together. In addition to keratinocytes, the stratum spinosum contains the immunologically active Langerhans cells.
Stratum Granulosum
The next layer above the stratum spinosum is the stratum granulosum. In this layer, keratinocytes have become nearly filled with keratin, giving their cytoplasm a granular appearance. Lipids are released by keratinocytes in this layer to form a lipid barrier in the epidermis. Cells in this layer have also started to die, because they are becoming too far removed from blood vessels in the dermis to receive nutrients. Each dying cell digests its own nucleus and organelles, leaving behind only a tough, keratin-filled shell.
Stratum Lucidum
Only on the palms of the hands and soles of the feet, the next layer above the stratum granulosum is the stratum lucidum. This is a layer consisting of stacks of translucent, dead keratinocytes that provide extra protection to the underlying layers.
Stratum Corneum
The uppermost layer of the epidermis everywhere on the body is the stratum corneum. This layer is made of flat, hard, tightly packed dead keratinocytes that form a waterproof keratin barrier to protect the underlying layers of the epidermis. Dead cells from this layer are constantly shed from the surface of the body. The shed cells are continually replaced by cells moving up from lower layers of the epidermis. It takes a period of about 48 days for newly formed keratinocytes in the stratum basale to make their way to the top of the stratum corneum to replace shed cells.
Functions of the Epidermis
The epidermis has several crucial functions in the body. These functions include protection, water retention, and vitamin D synthesis.
Protective Functions
The epidermis provides protection to underlying tissues from physical damage, pathogens, and UV light.
Protection from Physical Damage
Most of the physical protection of the epidermis is provided by its tough outer layer, the stratum corneum. Because of this layer, minor scrapes and scratches generally do not cause significant damage to the skin or underlying tissues. Sharp objects and rough surfaces have difficulty penetrating or removing the tough, dead, keratin-filled cells of the stratum corneum. If cells in this layer are pierced or scraped off, they are quickly replaced by new cells moving up to the surface from lower skin layers.
Protection from Pathogens

When pathogens such as viruses and bacteria try to enter the body, it is virtually impossible for them to enter through intact epidermal layers. Generally, pathogens can enter the skin only if the epidermis has been breached, for example by a cut, puncture, or scrape (like the one pictured in Figure 10.3.3). That’s why it is important to clean and cover even a minor wound in the epidermis. This helps ensure that pathogens do not use the wound to enter the body. Protection from pathogens is also provided by conditions at or near the skin surface. These include relatively high acidity (pH of about 5.0), low amounts of water, the presence of antimicrobial substances produced by epidermal cells, and competition with non-pathogenic microorganisms that normally live on the epidermis.
Protection from UV Light
UV light that penetrates the epidermis can damage epidermal cells. In particular, it can cause mutations in DNA that lead to the development of skin cancer, in which epidermal cells grow out of control. UV light can also destroy vitamin B9 (in forms such as folate or folic acid), which is needed for good health and successful reproduction. In a person with light skin, just an hour of exposure to intense sunlight can reduce the body’s vitamin B9 level by 50 per cent.
Melanocytes in the stratum basale of the epidermis contain small organelles called melanosomes, which produce, store, and transport the dark brown pigment melanin. As melanosomes become full of melanin, they move into thin extensions of the melanocytes. From there, the melanosomes are transferred to keratinocytes in the epidermis, where they absorb UV light that strikes the skin. This prevents the light from penetrating deeper into the skin, where it can cause damage. The more melanin there is in the skin, the more UV light can be absorbed.
Water Retention
Skin’s ability to hold water and not lose it to the surrounding environment is due mainly to the stratum corneum. Lipids arranged in an organized way among the cells of the stratum corneum form a barrier to water loss from the epidermis. This is critical for maintaining healthy skin and preserving proper water balance in the body.
Although the skin is impermeable to water, it is not impermeable to all substances. Instead, the skin is selectively permeable, allowing certain fat-soluble substances to pass through the epidermis. The selective permeability of the epidermis is both a benefit and a risk.
- Selective permeability allows certain medications to enter the bloodstream through the capillaries in the dermis. This is the basis of medications that are delivered using topical ointments, or patches (see Figure 10.3.4) that are applied to the skin. These include steroid hormones, such as estrogen (for hormone replacement therapy), scopolamine (for motion sickness), nitroglycerin (for heart problems), and nicotine (for people trying to quit smoking).
- Selective permeability of the epidermis also allows certain harmful substances to enter the body through the skin. Examples include the heavy metal lead, as well as many pesticides.
Vitamin D Synthesis
Vitamin D is a nutrient that is needed in the human body for the absorption of calcium from food. Molecules of a lipid compound named 7-dehydrocholesterol are precursors of vitamin D. These molecules are present in the stratum basale and stratum spinosum layers of the epidermis. When UV light strikes the molecules, it changes them to vitamin D3. In the kidneys, vitamin D3 is converted to calcitriol, which is the form of vitamin D that is active in the body.
What Gives Skin Its Colour?
Melanin in the epidermis is the main substance that determines the colour of human skin. It explains most of the variation in skin colour in people around the world. Two other substances also contribute to skin colour, however, especially in light-skinned people: carotene and hemoglobin.
- The pigment carotene is present in the epidermis and gives skin a yellowish tint, especially in skin with low levels of melanin.
- Hemoglobin is a red pigment found in red blood cells. It is visible through skin as a pinkish tint, mainly in skin with low levels of melanin. The pink colour is most visible when capillaries in the underlying dermis dilate, allowing greater blood flow near the surface.
Hear what Bill Nye has to say about the subject of skin colour in the video here.
Bacteria on Skin
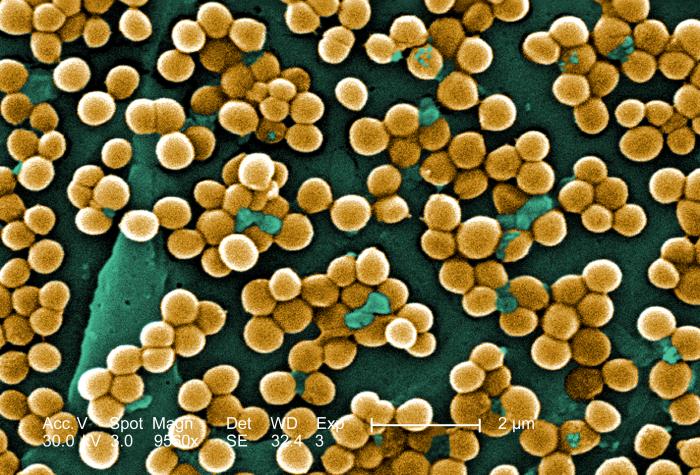
The surface of the human skin normally provides a home to countless numbers of bacteria. Just one square inch of skin normally has an average of about 50 million bacteria. These generally harmless bacteria represent roughly one thousand bacterial species (including the one in Figure 10.3.5) from 19 different bacterial phyla. Typical variations in the moistness and oiliness of the skin produce a variety of rich and diverse habitats for these microorganisms. For example, the skin in the armpits is warm and moist and often hairy, whereas the skin on the forearms is smooth and dry. These two areas of the human body are as diverse to microorganisms as rainforests and deserts are to larger organisms. The density of bacterial populations on the skin depends largely on the region of the skin and its ecological characteristics. For example, oily surfaces, such as the face, may contain over 500 million bacteria per square inch. Despite the huge number of individual microorganisms living on the skin, their total volume is only about the size of a pea.
In general, the normal microorganisms living on the skin keep one another in check, and thereby play an important role in keeping the skin healthy. If the balance of microorganisms is disturbed, however, there may be an overgrowth of certain species, and this may result in an infection. For example, when a patient is prescribed antibiotics, it may kill off normal bacteria and allow an overgrowth of single-celled yeast. Even if skin is disinfected, no amount of cleaning can remove all of the microorganisms it contains. Disinfected areas are also quickly recolonized by bacteria residing in deeper areas (such as hair follicles) and in adjacent areas of the skin.
Feature: Myth vs. Reality
Because of the negative health effects of excessive UV light exposure, it is important to know the facts about protecting the skin from UV light.
Myth |
Reality |
| “Sunblock and sunscreen are just different names for the same type of product. They both work the same way and are equally effective.” | Sunscreens and sunblocks are different types of products that protect the skin from UV light in different ways. They are not equally effective. Sunblocks are opaque, so they do not let light pass through. They prevent most of the rays of UV light from penetrating to the skin surface. Sunblocks are generally stronger and more effective than sunscreens. Sunblocks also do not need to be reapplied as often as sunscreens. Sunscreens, in contrast, are transparent once they are applied the skin. Although they can prevent most UV light from penetrating the skin when first applied, the active ingredients in sunscreens tend to break down when exposed to UV light. Sunscreens, therefore, must be reapplied often to remain effective. |
| “The skin needs to be protected from UV light only on sunny days. When the sky is cloudy, UV light cannot penetrate to the ground and harm the skin.” | Even on cloudy days, a significant amount of UV radiation penetrates the atmosphere to strike Earth’s surface. Therefore, using sunscreens or sunblocks to protect exposed skin is important even when there are clouds in the sky. |
| “People who have dark skin, such as African Americans, do not need to worry about skin damage from UV light.” | No matter what colour skin you have, your skin can be damaged by too much exposure to UV light. Therefore, even dark-skinned people should use sunscreens or sunblocks to protect exposed skin from UV light. |
| “Sunscreens with an SPF (sun protection factor) of 15 are adequate to fully protect the skin from UV light.” | Most dermatologists recommend using sunscreens with an SPF of at least 35 for adequate protection from UV light. They also recommend applying sunscreens at least 20 minutes before sun exposure and reapplying sunscreens often, especially if you are sweating or spending time in the water. |
| “Using tanning beds is safer than tanning outside in natural sunlight.” | The light in tanning beds is UV light, and it can do the same damage to the skin as the natural UV light in sunlight. This is evidenced by the fact that people who regularly use tanning beds have significantly higher rates of skin cancer than people who do not. It is also the reason that the use of tanning beds is prohibited in many places in people who are under the age of 18, just as youth are prohibited from using harmful substances, such as tobacco and alcohol. |
10.3 Summary
- The epidermis is the outer of the two main layers of the skin. It is very thin, but has a complex structure.
- Cell types in the epidermis include keratinocytes that produce keratin and make up 90 per cent of epidermal cells, melanocytes that produce melanin, Langerhans cells that fight pathogens in the skin, and Merkel cells that respond to light touch.
- The epidermis in most parts of the body consists of four distinct layers. A fifth layer occurs only in the epidermis of the palms of the hands and soles of the feet.
- The innermost layer of the epidermis is the stratum basale, which contains stem cells that divide to form new keratinocytes. The next layer is the stratum spinosum, which is the thickest layer and contains Langerhans cells and spiny keratinocytes. This is followed by the stratum granulosum, in which keratinocytes are filling with keratin and starting to die. The stratum lucidum is next, but only on the palms and soles. It consists of translucent dead keratinocytes. The outermost layer is the stratum corneum, which consists of flat, dead, tightly packed keratinocytes that form a tough, waterproof barrier for the rest of the epidermis.
- Functions of the epidermis include protecting underlying tissues from physical damage and pathogens. Melanin in the epidermis absorbs and protects underlying tissues from UV light. The epidermis also prevents loss of water from the body and synthesizes vitamin D.
- Melanin is the main pigment that determines the colour of human skin. The pigments carotene and hemoglobin, however, also contribute to skin colour, especially in skin with low levels of melanin.
- The surface of healthy skin normally is covered by vast numbers of bacteria representing about one thousand species from 19 phyla. Different areas of the body provide diverse habitats for skin microorganisms. Usually, microorganisms on the skin keep each other in check unless their balance is disturbed.
10.3 Review Questions
- What is the epidermis?
- Identify the types of cells in the epidermis.
- Describe the layers of the epidermis.
-
- State one function of each of the four epidermal layers found all over the body.
- Explain three ways the epidermis protects the body.
- What makes the skin waterproof?
- Why is the selective permeability of the epidermis both a benefit and a risk?
- How is vitamin D synthesized in the epidermis?
- Identify three pigments that impart colour to skin.
- Describe bacteria that normally reside on the skin, and explain why they do not usually cause infections.
- Explain why the keratinocytes at the surface of the epidermis are dead, while keratinocytes located deeper in the epidermis are still alive.
- Which layer of the epidermis contains keratinocytes that have begun to die?
-
- Explain why our skin is not permanently damaged if we rub off some of the surface layer by using a rough washcloth.
10.3 Explore More
Jonathan Eisen: Meet your microbes, TED, 2015.
Why Do We Blush?, SciShow, 2014.
The science of skin colour – Angela Koine Flynn, TED-Ed, 2016.
Attributions
Figure 10.3.1
Sunburn by QuinnHK at English Wikipedia on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 10.3.2
Blausen_0353_Epidermis by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 10.3.3
Isaac’s scraped knee close-up by Alpha on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
Figure 10.3.4
Nicoderm by RegBarc on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license. (No machine-readable author provided for original.)
Figure 10.3.5
Staphylococcus aureus bacteria, MRSA by Microbe World on Flickr is used under a CC BY-NC-SA 2.0 (https://creativecommons.org/licenses/by-nc-sa/2.0/) license.
References
Blausen.com staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Jeff Bone ‘n’ Pookie. (2020, July 19). Bill Nye the science guy explains we have different skin color. Youtube. https://www.youtube.com/watch?v=zOkj5jgC4sM&feature=youtu.be
SciShow. (2014, July 15). Why do we blush? YouTube. https://www.youtube.com/watch?v=9AcQXnOscQ8
TED. (2015, July 17). Jonathan Eisen: Meet your microbes. YouTube. https://www.youtube.com/watch?v=27lMmdmy-b8
TED-Ed. (2016, February 16). The science of skin color – Angela Koine Flynn. YouTube. https://youtu.be/_r4c2NT4naQ
The reddening of the skin that occurs when the outer layer of the skin is damaged by UV light from the sun or tanning lamps.
A form of electromagnetic radiation with wavelength shorter than that of visible light but longer than X-rays. UV radiation is present in sunlight, and constitutes about 10% of the total electromagnetic radiation output from the sun.
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.
The outer layer of skin that consists mainly of epithelial cells and lacks nerve endings, blood vessels, and other structures.
The major organ of the integumentary system that covers and protects the body and helps maintain homeostasis, for example, by regulating body temperature.
The inner layer of skin that is made of tough connective tissue and contains blood vessels, nerve endings, hair follicles, and glands.
Epithelial tissue that lines inner body surfaces and body openings and produces mucus.
The movement of a substance from an area of high concentration to an area of low concentration.
A tough, fibrous protein in skin, hair, and nails.
A type of epithelial cell found in the skin, hair, and nails that produces keratin.
A special skin cell that is responsible for producing melanin.
A cell found in the epidermis that functions as an antigen-presenting cell which binds antigens entering through the skin.
Oval-shaped mechanoreceptors essential for light touch sensation and found in the skin.
The innermost (deepest) layer of the epidermis. Consists of a single layer of columnar or cuboidal basal cells.
A thin, fibrous, extracellular matrix that separates the lining of an internal or external body surface from underlying connective tissue.
Found at the bottom of the epidermis — the outermost layer of skin. Basal cells produce new skin cells. As new skin cells are produced, they push older cells toward the skin's surface, where the old cells die and are sloughed off.
A layer of the epidermis found between the stratum granulosum and stratum basale. The main function of the stratum spinosum is to allow keratinocytes (cells that produce keratin) to mature.
A thin layer of cells in the epidermis. Keratinocytes migrating from the underlying stratum spinosum become known as granular cells in this layer. Function is to help to form a waterproof barrier that functions to prevent fluid loss from the body.
A substance that is insoluble in water. Examples include fats, oils and cholesterol. Lipids are made from monomers such as glycerol and fatty acids.
A central organelle containing hereditary material.
A tiny cellular structure that performs specific functions within a cell.
a thin, clear layer of dead skin cells in the epidermis named for its translucent appearance under a microscope. It is readily visible by light microscopy only in areas of thick skin, which are found on the palms of the hands and the soles of the feet.
The outer layer of the skin (epidermis). It serves as the primary barrier between the body and the environment.
Deoxyribonucleic acid - the molecule carrying genetic instructions for the development, functioning, growth and reproduction of all known organisms and many viruses.
A small organelle in a melanocyte that synthesizes, stores, and transports melanin.
A brown pigment produced by melanocytes in the skin that gives skin most of its color and prevents UV light from penetrating the skin.
A membrane which allows the passage of some molecules or ions and inhibits the passage of others. The capacity to filter molecular transport in this manner is called selective permeability.
The female sex hormone secreted mainly by the ovaries.
A pigment in the epidermis that gives skin a yellowish tint, especially in skin with low levels of melanin.
An oxygen-binding protein containing iron that is the principal component of red blood cells.
A microorganism which causes disease.
Any member of a large group of unicellular microorganisms which have cell walls but lack organelles and an organized nucleus, including some which can cause disease.

