151 17.7 Case Study Conclusion: Defending Your Defenses
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study Conclusion: Defending Your Defenses
These people are participating in a bike ride to raise funds for leukemia and lymphoma research (Figure 17.7.1). Leukemia and lymphoma are blood cancers. In 2020, approximately 6,900 Canadians will be diagnosed with leukemia and 3,000 will die from this cancer. Lymphoma is the most common type of blood cancer. As a lymphoma patient, Hakeem, who you learned about in the beginning of this chapter, may eventually benefit from research funded by a bike ride like this one.
What type of blood cell is affected in lymphoma? As the name implies, lymphoma is a cancer that affects lymphocytes, which are a type of leukocyte. As you have learned in this chapter, there are different types of lymphocytes, including the B and T cells of the adaptive immune system. Different types of lymphoma affect different types of lymphocytes in different ways. It is important to correctly identify the type of lymphoma, so that patients can be treated appropriately.
You may recall that one of Hakeem’s symptoms was a swollen lymph node, and he was diagnosed with lymphoma after a biopsy of that lymph node. Swollen lymph nodes are a common symptom of lymphoma. As you have learned, lymph nodes are distributed throughout the body along lymphatic vessels, as part of the lymphatic system. The lymph nodes filter lymph and store lymphocytes. Therefore, they play an important role in fighting infections. Because of this, they will often swell in response to an infection. In Hakeem’s case, the swelling and other symptoms did not improve after several weeks and a course of antibiotics, which caused Dr. Hayes to suspect lymphoma instead. The biopsy showed that Hakeem did indeed have cancerous lymphocytes in his lymph nodes.
But which type of lymphocytes were affected? Lymphoma most commonly affects B or T lymphocytes. The two major types of lymphoma are called Hodgkin (HL) or non-Hodgkin lymphoma (NHL). NHL is more common than HL. In 2020, the Canadian Cancer Society estimates 10,400 Canadians will be diagnosed with non-Hodgkin lymphoma, whereas 1,000 will be diagnosed with Hodgkin lymphoma. While HL is one distinct type of lymphoma, NHL has about 60 different subtypes, depending on which specific cells are affected and how.
Hakeem was diagnosed with a type of NHL called diffuse large B-cell lymphoma (DLBCL) — the most common type of NHL. This type of lymphoma affects B cells and causes them to appear large under the microscope. In addition to Hakeem’s symptoms of fatigue, swollen lymph nodes, loss of appetite, and weight loss, common symptoms of this type of lymphoma include fever and night sweats. It is an aggressive and fast-growing type of lymphoma that is fatal if not treated. The good news is that with early detection and proper treatment, about 70% of patients with DLBCL can be cured.
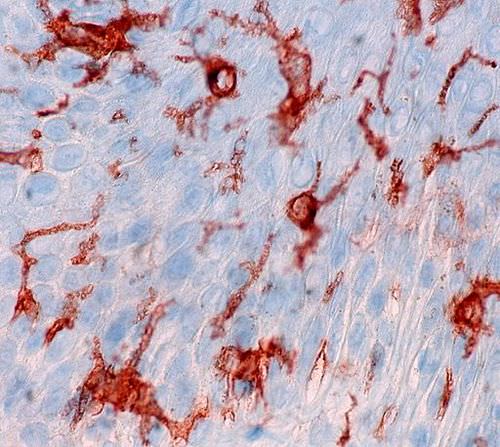
How do physicians determine the specific type of lymphoma? Tissue obtained from a biopsy can be examined under a microscope to observe physical changes (such as abnormal cell size or shape) that are characteristic of a particular subtype of lymphoma. Additionally, tests can be performed on the tissue to determine which cell-surface antigens are present. Recall that antigens are molecules that bind to specific antibodies. Antibodies can be produced in the laboratory and labeled with compounds that can be identified by their colour under a microscope. When these antibodies are applied to a tissue sample, this colour will appear wherever the antigen is present, because it binds to the antibody. This technique was used in the photomicrograph in Figure 17.7.2 to identify the presence of a cell-surface antigen (shown as reddish-brown) in a sample of skin cells. This technique, called immunohistochemistry, is also commonly used to identify antigens in tissue samples from lymphoma patients.
Why would identifying cell-surface antigens be important in diagnosing and treating lymphoma? As you have learned, the immune system uses antigens present on the surface of cells or pathogens to distinguish between self and non-self, and to launch adaptive immune responses. Cells that become cancerous often change their cell-surface antigens. This is one way that the immune system can identify and destroy them. Also, different cell types in the body can sometimes be identified by the presence of specific cell-surface antigens. Knowing the types of cell-surface antigens present in a tissue sample can help physicians identify which cells are cancerous, and possibly the specific subtype of cancer. Knowing this information can be helpful in choosing more tailored and effective treatments.
One treatment for NHL is, in fact, the use of medications made from antibodies that bind to cell-surface antigens present on cells affected by the specific subtype of NHL. This is called immunotherapy. These drugs can directly bind to and kill the cancerous cells. For patients with DLBCL like Hakeem, immunotherapy is often used in conjunction with chemotherapy and radiation as a course of treatment. Although Hakeem has a difficult road ahead, he and his medical team are optimistic that — given the high success rate when DLBCL is caught and treated early — he may be cured. More research into how the immune system functions may lead to even better treatments for lymphoma — and other types of cancers — in the future.
Chapter 17 Summary
In this chapter, you learned about the immune system. Specifically, you learned that:
- Any agent that can cause disease is called a pathogen. Most human pathogens are microorganisms, such as bacteria and viruses. The immune system is the body system that defends the human host from pathogens and cancerous cells.
- The innate immune system is a subset of the immune system that provides very quick, but non-specific responses to pathogens. It includes multiple types of barriers to pathogens, leukocytes that phagocytize pathogens, and several other general responses.
- The adaptive immune system is a subset of the immune system that provides specific responses tailored to particular pathogens. It takes longer to put into effect, but it may lead to immunity to the pathogens.
- Both innate and adaptive immune responses depend on the ability of the immune system to distinguish between self and non-self molecules. Most body cells have major histocompatibility complex (MHC) proteins that identify them as self. Pathogens, infected cells, and tumor cells have non-self proteins called antigens that the immune system recognizes as foreign.
- Antigens are proteins that bind to specific receptors on immune system cells and elicit an adaptive immune response. Some immune cells (B cells) respond to foreign antigens by producing antibodies that bind with antigens and target pathogens for destruction.
- An important role of the immune system is tumor surveillance. Killer T cells of the adaptive immune system find and destroy tumor cells, which they can identify from their abnormal antigens.
- The neuroimmune system that protects the central nervous system is thought to be distinct from the peripheral immune system that protects the rest of the human body. The blood-brain and blood-spinal cord barriers are one type of protection of the neuroimmune system. Neuroglia also play a role in this system, for example, by carrying out phagocytosis.
- The lymphatic system is a human organ system that is a vital part of the adaptive immune system. It consists of several organs and a system of vessels that transport or filter the fluid called lymph. The main immune function of the lymphatic system is to produce, mature, harbor, and circulate white blood cells called lymphocytes, which are the main cells in the adaptive immune system, and are circulated in lymph.
-
- The return of lymph to the bloodstream is one of the functions of the lymphatic system. Lymph flows from tissue spaces, where it leaks out of blood vessels, to major veins in the upper chest. It is then returned to the cardiovascular system. Lymph is similar in composition to blood plasma. Its main cellular components are lymphocytes.
- Lymphatic vessels called lacteals are found in villi that line the small intestine. Lacteals absorb fatty acids from the digestion of lipids in the digestive system. The fatty acids are then transported through the network of lymphatic vessels to the bloodstream.
- Lymphocytes, which include B cells and T cells, are the subset of leukocytes involved in adaptive immune responses. They may create a lasting memory of and immunity to specific pathogens.
- All lymphocytes are produced in bone marrow and then go through a process of maturation, in which they “learn” to distinguish self from non-self. B cells mature in the bone marrow, and T cells mature in the thymus. Both the bone marrow and thymus are considered primary lymphatic organs.
- Secondary lymphatic organs include the tonsils, spleen, and lymph nodes. There are four pairs of tonsils that encircle the throat. The spleen filters blood, as well as lymph. There are hundreds of lymph nodes located in clusters along the lymphatic vessels. All of these secondary organs filter lymph and store lymphocytes, so they are sites where pathogens encounter and activate lymphocytes and initiate adaptive immune responses.
- Unlike the adaptive immune system, the innate immune system does not confer immunity. The innate immune system includes surface barriers, inflammation, the complement system, and a variety of cellular responses.
-
- The body’s first line of defense consists of three different types of barriers that keep most pathogens out of body tissues. The types of barriers are mechanical, chemical, and biological barriers.
-
-
- Mechanical barriers — which include the skin, mucous membranes, and fluids (such as tears and urine) — physically block pathogens from entering the body.
- Chemical barriers — such as enzymes in sweat, saliva, and semen — kill pathogens on body surfaces.
- Biological barriers are harmless bacteria that use up food and space so pathogenic bacteria cannot colonize the body.
- If pathogens breach the protective barriers, inflammation occurs. This creates a physical barrier against the spread of infection and repairs tissue damage. Inflammation is triggered by chemicals (such as cytokines and histamines), and it causes swelling, redness, and warmth.
- The complement system is a complex biochemical mechanism that helps antibodies kill pathogens. Once activated, the complement system consists of more than two dozen proteins that lead to disruption of the cell membrane of pathogens and bursting of the cells.
- Cellular responses of the innate immune system involve various types of leukocytes (white blood cells). For example, neutrophils, macrophages, and dendritic cells phagocytize pathogens. Basophils and mast cells release chemicals that trigger inflammation. Natural killer cells destroy cancerous or virus-infected cells, and eosinophils kill parasites.
- Many pathogens have evolved mechanisms that help them evade the innate immune system. For example, some pathogens form a protective capsule around themselves, and some mimic host cells so the immune system does not recognize them as foreign.
-
- The main cells of the adaptive immune system are lymphocytes. There are two major types of lymphocytes: T cells and B cells. Both types must be activated by foreign antigens to become functioning immune cells.
-
- Most activated T cells become either killer T cells or helper T cells. Killer T cells destroy cells that are infected with pathogens or are cancerous. Helper T cells manage immune responses by releasing cytokines that control other types of leukocytes.
- Activated B cells form plasma cells that secrete antibodies, which bind to specific antigens on pathogens or infected cells. The antibody-antigen complexes generally lead to the destruction of the cells, for example, by attracting phagocytes or triggering the complement system.
- After an adaptive immune response occurs, long-lasting memory B cells and memory T cells may remain to confer immunity to the specific pathogen that caused the adaptive immune response. These memory cells are ready to activate an immediate response if they are exposed to the same antigen again in the future.
- Immunity may be active or passive.
-
- Active immunity occurs when the immune system has been presented with antigens that elicit an adaptive immune response. This may occur naturally as the result of an infection, or artificially as the result of immunization. Active immunity may last for years or even for life.
- Passive immunity occurs without an adaptive immune response by the transfer of antibodies or activated T cells. This may occur naturally between a mother and her fetus or her nursing infant, or it may occur artificially by injection. Passive immunity lasts only as long as the antibodies or activated T cells remain alive in the body, generally just weeks or months.
- Many pathogens have evolved mechanisms to evade the adaptive immune system. For example, human immunodeficiency virus (HIV) evades the adaptive immune system by frequently changing its antigens and by forming its outer envelope from the host’s cell membrane.
- An allergy is a disorder in which the immune system makes an inflammatory response to a harmless antigen. Any antigen that causes allergies is called an allergen. Common allergens include pollen, dust mites, mold, specific foods (such as peanuts), insect stings, and certain medications (such as aspirin).
-
- The prevalence of allergies has been increasing for decades, especially in developed countries, where they are much more common than in developing countries. The hygiene hypothesis posits that this has occurred because humans evolved to cope with more pathogens than we now typically face in our relatively sterile environments in developed countries. As a result, the immune system “keeps busy” by attacking harmless antigens.
- Allergies occur when B cells are first activated to produce large amounts of antibodies to an otherwise harmless allergen, and the antibodies attach to mast cells. On subsequent exposures to the allergen, the mast cells immediately release cytokines and histamines that cause inflammation.
- Mild allergy symptoms are frequently treated with antihistamines that counter histamines and reduce allergy symptoms. A severe systemic allergic reaction, called anaphylaxis, is a medical emergency that is usually treated with injections of epinephrine. Immunotherapy for allergies involves injecting increasing amounts of allergens to desensitize the immune system to them.
- Autoimmune diseases occur when the immune system fails to recognize the body’s own molecules as self and attacks them, causing damage to tissues and organs. A family history of autoimmunity and female gender are risk factors for autoimmune diseases.
-
- In some autoimmune diseases, such as type I diabetes, the immune system attacks and damages specific body cells. In other autoimmune diseases, such as systemic lupus erythematosus, many different tissues and organs may be attacked and injured. Autoimmune diseases generally cannot be cured, but their symptoms can often be managed with drugs or other treatments.
- Immunodeficiency occurs when the immune system is not working properly, generally because one or more of its components are inactive. As a result, the immune system is unable to fight off pathogens or cancers that a normal immune system would be able to resist.
-
- Primary immunodeficiency is present at birth and caused by rare genetic diseases. An example is severe combined immunodeficiency. Secondary immunodeficiency occurs because of some event or exposure experienced after birth. Possible causes include substance abuse, obesity, and malnutrition, among others.
- The most common cause of immunodeficiency in the world today is human immunodeficiency virus (HIV), which infects and destroys helper T cells. HIV is transmitted through mucous membranes or body fluids. The virus may eventually lead to such low levels of helper T cells that opportunistic infections occur. When this happens, the patient is diagnosed with acquired immunodeficiency syndrome (AIDS). Medications can control the multiplication of HIV in the human body, but it can’t eliminate the virus completely.
Up to this point, this book has covered body systems that carry out processes within individuals, such as the digestive, muscular, and immune systems. Read the next chapter to learn about the body system that allows humans to produce new individuals — the reproductive system.
Chapter 17 Review
-
- Compare and contrast a pathogen and an allergen.
- Describe three ways in which pathogens can enter the body.
- The complement system involves the activation of several proteins to kill pathogens. Why do you think this is considered part of the innate immune system, instead of the adaptive immune system?
- Why are innate immune responses generally faster than adaptive immune responses?
- Explain how an autoimmune disease could be triggered by a pathogen.
- What is an opportunistic infection? Name two diseases or conditions that could result in opportunistic infections. Explain your answer.
- Which cell type in the immune system can be considered an “antibody factory?”
- Besides foreign pathogens, what is one thing that the immune system protects the body against?
- What cell type in the immune system is infected and killed by HIV?
- Name two types of cells that produce cytokines in the immune system. What are two functions of cytokines in the immune system?
- Many pathogens evade the immune system by altering their outer surface in some way. Based on what you know about the functioning of the immune system, why is this often a successful approach?
- What is “missing self?” How does this condition arise?
17.7 Explore More
What is leukemia? – Danilo Allegra and Dania Puggioni, TED-Ed, 2015.
Attributions
Figure 17.7.1
Cycling to Beat Blood Cancer by Blood Cancer UK (Formerly Bloodwise) on Flickr is used under a CC BY-NC-ND 2.0 (https://creativecommons.org/licenses/by-nc-nd/2.0/) license.
Figure 17.7.2
antigen stain by Ed Uthman from Houston, TX, USA on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
References
Hodgkin lymphoma statistics [online article]. (2020). Canadian Cancer Society. https://www.cancer.ca:443/en/cancer-information/cancer-type/hodgkin-lymphoma/statistics/?region=on
Non-Hodgkin lymphoma statistics [online article]. (2020). Canadian Cancer Society. https://www.cancer.ca:443/en/cancer-information/cancer-type/non-hodgkin-lymphoma/statistics/?region=on
TED-Ed. (2015, April 30). What is leukemia? – Danilo Allegra and Dania Puggioni. YouTube. https://www.youtube.com/watch?v=Z3B-AaqjyjE&feature=youtu.be
A cancer that begins in infection-fighting cells of the immune system, called lymphocytes.
A subset of the immune system that makes tailored attacks against specific pathogens or tumor cells such as the production of antibodies that match specific antigens.
One of many small structures located along lymphatic vessels where pathogens are filtered from lymph and destroyed by lymphocytes.
A body system consisting of a network of tissues and organs that help rid the body of toxins, waste and other unwanted materials. The primary function of the lymphatic system is to transport lymph, a fluid containing infection-fighting white blood cells, throughout the body.
A fluid that leaks out of capillaries into spaces between cells and circulates in the vessels of the lymphatic system.
A type of white blood cell and, specifically, a type of lymphocyte.
Many B cells mature into what are called plasma cells that produce antibodies (proteins) necessary to fight off infections while other B cells mature into memory B cells.
An antibody, also known as an immunoglobulin, is a large, Y-shaped protein produced mainly by plasma cells that is used by the immune system to neutralize pathogens such as pathogenic bacteria and viruses.
A treatment for an allergy in which a patient is gradually desensitized to an allergen through periodic injections with increasing amounts of the allergen; or treatment for cancer that attempts to stimulate the immune system to destroy cancer cells.
The treatment of disease by the use of chemical substances, especially the treatment of cancer by cytotoxic (cell-killing) and other drugs.
A microorganism which causes disease.
An organisms that is so small it is invisible to the human eye.
Any member of a large group of unicellular microorganisms which have cell walls but lack organelles and an organized nucleus, including some which can cause disease.
A tiny, nonliving particle that contains nucleic acids but lacks other characteristics of living cells and may cause human disease.
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.
A subset of the immune system that makes generic attacks such as inflammation against invading pathogens.
The state of being immune from or insusceptible to a particular disease or the like. the condition that permits either natural or acquired resistance to disease. the ability of a cell to react immunologically in the presence of an antigen.
A set of molecules normally found on most human cells that provide a way for the immune system to recognize body cells as self.
Molecules on the surface of cells or viruses that the immune system identifies as either self (produced by your own body) or non-self (not produced by your own body).
A T lymphocyte (a type of white blood cell), also known as a cytoxic T cell) that kills cancer cells, cells that are infected (particularly with viruses), or cells that are damaged in other ways.
A part of the immune system that protects the central nervous system.
One of two main divisions of the nervous system that includes the brain and spinal cord.
The part of the immune system that protects all of the body except for the central nervous system (which is protected by the neuroimmune system).
The process by which a cell uses its plasma membrane to engulf a large particle, giving rise to an internal compartment called the phagosome.
Refers to the body system consisting of the heart, blood vessels and the blood. Blood contains oxygen and other nutrients which your body needs to survive. The body takes these essential nutrients from the blood.
A straw-yellow fluid part of blood that contains many dissolved substances and blood cells.
A lymphatic capillary that absorbs dietary fats in the villi of the small intestine.
A microscopic, finger-like projections in a mucous membrane that form a large surface area for absorption.
A long, narrow, tube-like organ of the digestive system where most chemical digestion of food and virtually all absorption of nutrients take place.
A body system including a series of hollow organs joined in a long, twisting tube from the mouth to the anus. The hollow organs that make up the GI tract are the mouth, esophagus, stomach, small intestine, large intestine, and anus. The liver, pancreas, and gallbladder are the solid organs of the digestive system.
A type of lymphocyte that kills infected or cancerous cells (killer T cell) or helps regulate the immune response (helper T cell).
A soft connective tissue in spongy bone that produces blood cells.
An organ of the lymphatic system where lymphocytes called T cells mature.
Any organ where lymphocytes are formed and mature. They provide an environment for stem cells to divide and mature into B- and T- cells: There are two primary lymphatic organs: the red bone marrow and the thymus gland.
A set of organs which includes lymph nodes and the spleen) maintain mature naive lymphocytes and initiate an adaptive immune response.
An organ of the lymphatic system where lymphocytes called T cells mature.
A secondary organ of the lymphatic system where blood and lymph are filtered.
A physical barrier which pathogens cannot cross, protecting the body. These barriers include: The outer layer of the skin and mucous membranes.
The major organ of the integumentary system that covers and protects the body and helps maintain homeostasis, for example, by regulating body temperature.
Epithelial tissue that lines inner body surfaces and body openings and produces mucus.
A liquid waste product of the body that is formed by the kidneys and excreted by the other organs of the urinary system.
Salty fluid secreted into ducts by sweat glands in the dermis that excretes wastes and helps cool the body; also called perspiration.
A fluid secreted by salivary glands that keeps the mouth moist and contains the digestive enzymes amylase and lipase.
Fluid containing sperm and glandular secretions, which nourishes sperm and carries them through the urethra and out of the body.
The response of the innate immune system that establishes a physical barrier against the spread of infection and repairs tissue damage while causing redness, swelling, and warmth.
A chemical released by injured, infected, or immune cells that triggers inflammation or other immune responses.
A compound which is released by cells in response to injury and in allergic and inflammatory reactions, causing contraction of smooth muscle and dilation of capillaries.
An innate immune response that consists of a cascade of proteins that complement the killing of pathogens by antibodies.
The semipermeable membrane surrounding the cytoplasm of a cell.
A type of immune cell that is one of the first cell types to travel to the site of an infection. Neutrophils help fight infection by ingesting microorganisms and releasing enzymes that kill the microorganisms. A neutrophil is a type of white blood cell, a type of granulocyte, and a type of phagocyte.
A large phagocytic cell found in stationary form in the tissues or as a mobile white blood cell, especially at sites of infection.
A special type of immune cell that is found in tissues, such as the skin, and boosts immune responses by showing antigens on its surface to other cells of the immune system. A dendritic cell is a type of phagocyte and a type of antigen-presenting cell (APC).
A type of immune cell that has granules (small particles) with enzymes that are released during allergic reactions and asthma. A basophil is a type of white blood cell and a type of granulocyte.
A type of white blood cell found in connective tissues all through the body, especially under the skin, near blood vessels and lymph vessels, in nerves, and in the lungs and intestines. Mast cells play an important role in how the immune system responds to certain pathogens by releasing chemicals such as histamines and cytokines during allergic reactions and certain immune responses.
A type of immune cell that has granules (small particles) with enzymes that can kill tumor cells or cells infected with a virus. A natural killer cell is a type of white blood cell.
A type of immune cell that has granules (small particles) with enzymes that are released during infections, allergic reactions, and asthma. An eosinophil is a type of white blood cell and a type of granulocyte.
A type of leukocyte produced by the lymphatic system that is a key cell in the adaptive immune response to a specific pathogen or tumor cell.
A type of immune cell that stimulates killer T cells, macrophages, and B cells to make immune responses. A helper T cell is a type of white blood cell and a type of lymphocyte.
A fully differentiated B cell that produces a single type of antibody.
A lymphocyte (B or T cell) that retains a “memory” of a specific pathogen after an infection is over and thus provides immunity to the pathogen.
The ability to resist a specific pathogen that results when an adaptive immune response to the pathogen produces memory lymphocytes for that pathogen.
Short-term immunity to a particular pathogen that results when antibodies or activated T cells are transferred to a person who has never been exposed to the pathogen.
Either of two species of Lentivirus that infect humans. Over time, they cause acquired immunodeficiency syndrome, a condition in which progressive failure of the immune system allows life-threatening opportunistic infections and cancers to thrive.
A damaging immune response by the body to a substance, especially pollen, fur, a particular food, or dust, to which it has become hypersensitive.
Any substance, typically an antigen, that causes an allergy.
An acute, potentially life-threatening hypersensitivity reaction, involving the release of mediators from mast cells, basophils and recruited inflammatory cells. Anaphylaxis is defined by a number of signs and symptoms, alone or in combination, which occur within minutes, or up to a few hours, after exposure to a provoking agent. It can be mild, moderate to severe, or severe. Most cases are mild but any anaphylaxis has the potential to become life-threatening.
A type of disease, such as Type 1 Diabetes, in which the immune system attacks the body’s own cells as though they were pathogens.
A group of more than 400 rare, chronic disorders in which part of the body’s immune system is missing or functions improperly. While not contagious, these diseases are caused by hereditary or genetic defects, and, although some disorders present at birth or in early childhood, the disorders can affect anyone, regardless of age or gender.
Occurs when the immune system is compromised due to an environmental factor. Examples of these outside forces include HIV, chemotherapy, severe burns or malnutrition.
The late stage of HIV infection that occurs when the body's immune system is badly damaged because of the virus.

