162 18.11 Contraception
Created by CK-12 Foundation/Adapted by Christine Miller

Family Planning Pioneer
Her name was Marie Stopes, and she was a British author and paleobotanist who lived from 1880 to 1958. She is pictured in Figure 18.11.1 in her lab next to her microscope. Stopes made significant contributions to science and was the first woman on the faculty of the University of Manchester in England. Her primary claim to fame was her work as a family planning pioneer.
Along with her husband, Stopes founded the first birth control clinic in Britain. She also edited a newsletter called Birth Control News, which gave explicit practical advice on how to avoid unwanted pregnancies. In 1918, she published a sex manual titled Married Love. The book was controversial and influential, bringing the subject of contraception into wide public discourse for the first time.
What Is Contraception?
About a century after Married Love, more than half of all fertile married couples worldwide use some form of contraception. Contraception, also known as birth control, is any method or device used to prevent pregnancy. Birth control methods have been used for centuries, but safe and effective methods only became available in the 20th century, in part because of the work of people like Marie Stopes.
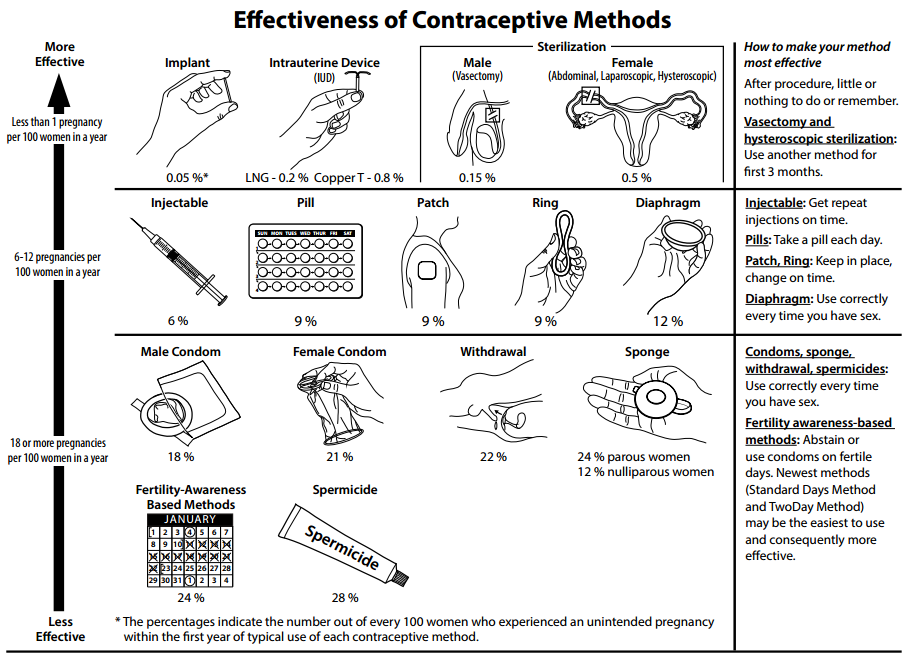
Many different birth control methods are currently available, but they differ considerably in their effectiveness at preventing pregnancy. The effectiveness of contraception is generally expressed as the failure rate, which is the percentage of women who become pregnant using a given method during the first year of use. Virtually no one uses any method of birth control perfectly, so the failure rate with typical use is almost always higher — and often much higher — than the failure rate with perfect use. For example, with perfect use, a birth control method might have a failure rate of just 1%, whereas with typical use, the failure rate might be 25%. For comparison, there is an average one-year pregnancy rate of 85% if no contraception is used.
All methods of birth control have potential adverse effects, but their health risks are less than the health risks associated with pregnancy. Using contraception to space the children in a family is also good for the children’s health and development, as well as for the health of the mother.
Types of Contraception and Their Effectiveness
Types of birth control methods include barrier methods, hormonal methods, intrauterine devices, behavioural methods, and sterilization. With the exception of sterilization, all of these methods are reversible. Examples of each type of birth control method and their failure rates with typical use are described below. Much of the information is also summarized in Figure 18.11.2.
Barrier Methods
Barrier methods are devices that are used to physically block sperm from entering the uterus. They include condoms and diaphragms.

Condoms
Condoms are the most commonly used method of birth control globally. There are condoms for females and males, but male condoms are more widely used, less expensive, and more readily available. Both types of condoms are pictured in Figures 18.11.3 and 18.11.4. A male condom is placed on a man’s erect penis, and a female condom is placed inside a woman’s vagina. Whichever type of condom is used, it must be put in place before sexual intercourse occurs. Condoms work by physically blocking ejaculated sperm from entering the vagina of the sexual partner. With typical use, male condoms have an 18% failure rate, and female condoms have a 21% failure rate. Unlike virtually all other birth control methods, condoms also help prevent the spread of sexually transmitted infections (STIs), in addition to helping to prevent pregnancy.


Diaphragms
Diaphragms, like the one pictured in Figure 18.11.5, ideally prevent sperm from passing through the cervical canal and into the uterus. A diaphragm is inserted vaginally before sexual intercourse occurs and must be placed over the cervix to be effective. It is usually recommended that a diaphragm be covered with spermicide before insertion for extra protection. It is also recommended that the diaphragm be left in place for at least six hours after intercourse. The failure rate of diaphragms with typical use is about 12%, which is about half that of condoms. However, diaphragms do not help prevent the spread of STIs, and their use is also associated with an increased frequency of urinary tract infections in females.
Hormonal Methods
Hormonal contraception is the administration of hormones to prevent ovulation. Hormones can be taken orally in birth control pills, implanted under the skin, injected into a muscle, or received transdermally from a skin patch. Hormonal methods are currently available only for women, although hormonal contraceptives for men are being tested in clinical trials.
Birth control pills are the most common form of hormonal contraception. There are two types of pills: the combined pill (which contains both estrogen and progesterone) and the progesterone-only pill. Both types of pills inhibit ovulation and thicken cervical mucus. The failure rate of birth control pills is only about 1% or less, if used perfectly. However, the failure rate rises to about 10% with typical use, because women do not always remember to take the pill at the same time every day. The combined pill is associated with a slightly increased risk of blood clots, but a reduced risk of ovarian and endometrial cancers. The progesterone-only pill does not increase the risk of blood clots, but it may cause irregular menstrual periods. It may take a few weeks or even months for fertility to return to normal after long-term use of birth control pills.
Intrauterine Devices
An intrauterine device (IUD) is a T-shaped or coiled plastic structure that is inserted into the uterus via the vagina and cervix that contains either copper or a hormone. You can see an IUD in the uterus in the drawing of the female reproductive system in Figure 18.11.6. An IUD is inserted by a physician and may be left in place for months or even years. A physician also must remove an IUD, using the strings attached to the device. The copper in copper IUDs prevents pregnancy by interfering with the movement of sperm so they cannot reach and fertilize an egg. The copper may also prevent implantation in the unlikely circumstance of a sperm managing to reach and fertilize an ovum, in which case the blastocyst/zygote would be shed during menstruation. The hormones in hormonal IUDs prevent pregnancy by thickening cervical mucus and trapping sperm. The hormones may also interfere with ovulation, so there is no egg to fertilize.
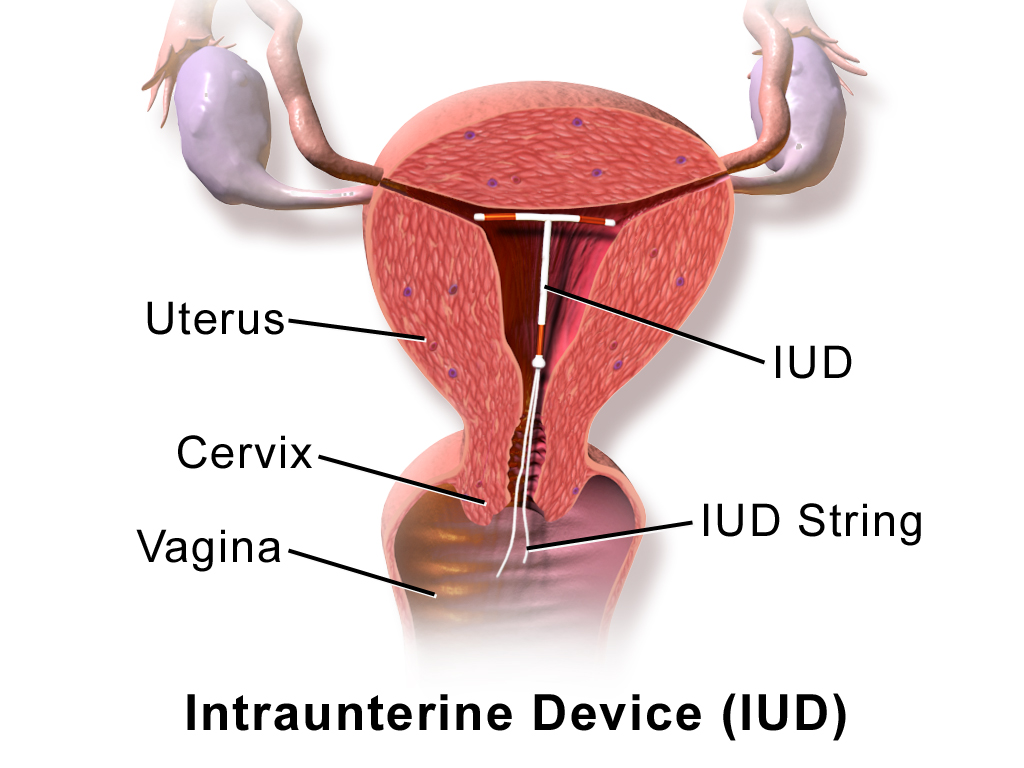
For both types of IUDs, the failure rates are <1%, and failure rates with typical use are virtually the same as failure rates with perfect use. Their effectiveness is one reason that IUDs are among the most widely used forms of reversible contraception. Once removed, even after long-term use, fertility returns to normal immediately. On the other hand, IUDs do have a risk of complications, including increased menstrual bleeding and more painful menstrual cramps. IUDs are also occasionally expelled from the uterus, and there is a slight risk of perforation of the uterus by the IUD.
Behavioural Methods
The least effective methods of contraception are behavioural methods. They involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present. Behavioural methods include fertility awareness methods and withdrawal. Abstinence from sexual activity, or at least from vaginal intercourse, is sometimes considered a behavioural method, as well — but it is unlikely to be practiced consistently enough by most people to prevent pregnancy. Even teens who receive abstinence-only sex education do not have reduced rates of pregnancy. Abstinence is also ineffective in cases of non-consensual sex.
Fertility Awareness Methods
Fertility awareness methods involve estimating the most fertile days of the menstrual cycle and then avoiding unprotected vaginal intercourse on those days. The most fertile days are generally a few days before ovulation occurs, the day of ovulation, and another day or two after that. Unless unprotected sex occurs on those days, pregnancy is unlikely. Techniques for estimating the most fertile days include monitoring and detecting minor changes in basal body temperature or cervical secretions. This requires daily motivation and diligence, so it is not surprising that typical-use failure rates of these methods are at least 20–25%, and for some individuals may be as high as using no contraception at all (85%).
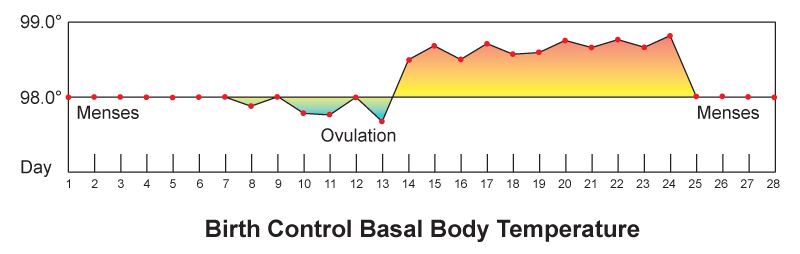
Basal body temperature is the lowest body temperature when the body is at rest (usually during sleep). It is most often estimated by a temperature measurement taken immediately upon awakening in the morning and before any physical activity has occurred. Basal body temperature normally rises after ovulation occurs, as shown in the graph below (Figure 18.11.7). The increase in temperature is small but consistent and may be used to determine when ovulation occurs, around which time unprotected intercourse should be avoided to prevent pregnancy. However, basal body temperature only shows when ovulation has already occurred, and it cannot predict in advance when ovulation will occur. Sperm can live for up to a week in the female reproductive tract, so determining the occurrence of ovulation only after ovulation has already happened is a major drawback of this method.
Monitoring cervical mucus has the potential for being more effective than monitoring basal body temperature, because it can predict ovulation ahead of time. As ovulation approaches, cervical secretions usually increase in amount and become thinner (which helps sperm swim through the cervical canal). By recognizing the changing characteristics of cervical mucus, a woman may be able to predict when she will ovulate. From this information, she can determine when she should avoid unprotected sex to prevent pregnancy.
Withdrawal
Withdrawal (also called coitus interruptus) is the practice of withdrawing the penis from the vagina before ejaculation ensues. The main risk of the withdrawal method is that the man may not perform the maneuver correctly or in a timely manner. Fluid typically released from the penis before ejaculation occurs may also contain some sperm. In addition, if sperm are ejaculated just outside of the vagina, there is a chance they will be able to enter the vagina and travel through the female reproductive tract to fertilize an egg. For all these reasons, the withdrawal method has a relatively high failure rate of about 22% with typical use.
Sterilization
The most effective contraceptive method is sterilization. In both sexes, sterilization generally involves surgical procedures that are considered irreversible. Additional surgery may be able to reverse a sterilization procedure, but there are no guarantees. Male sterilization is generally less invasive and less risky than female sterilization.
Male Sterilization
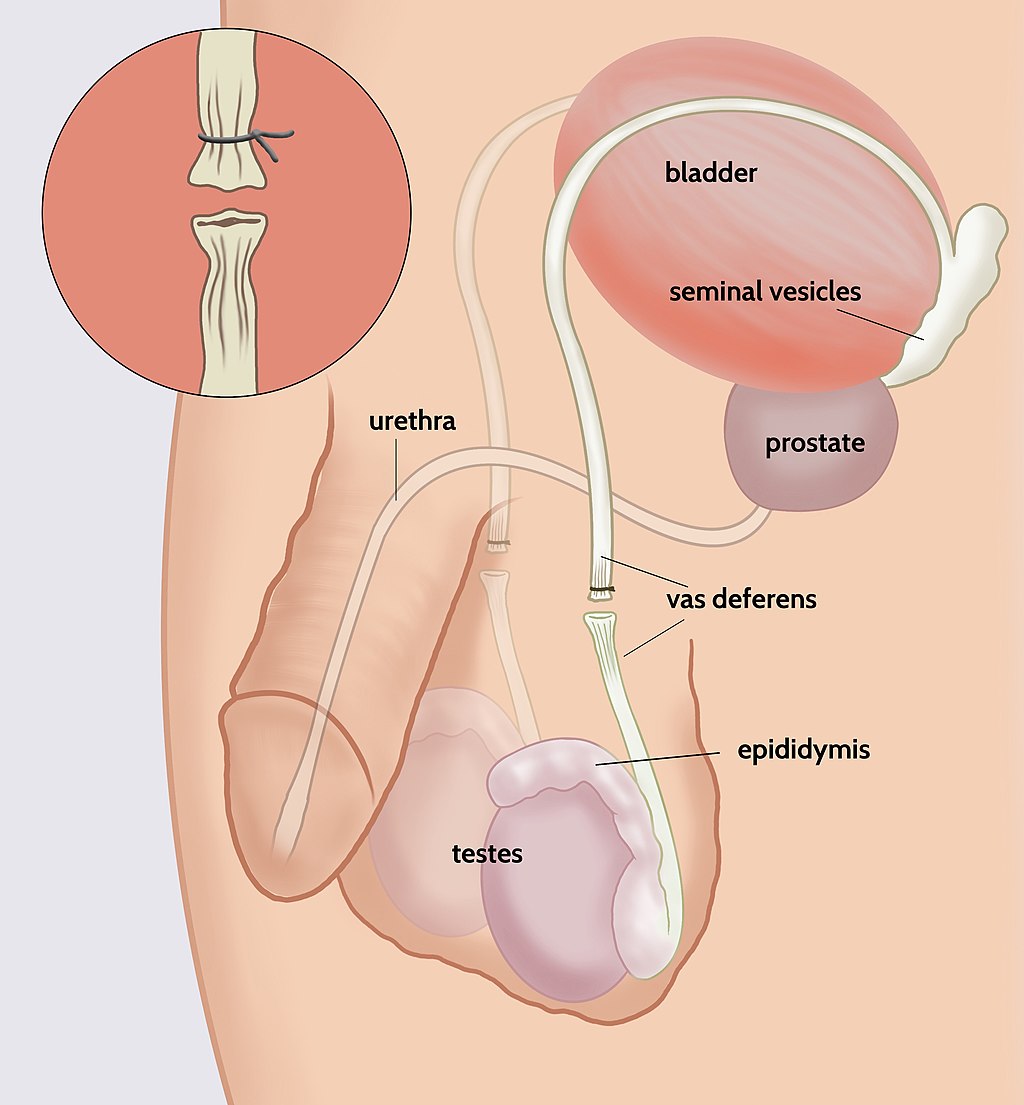
Male sterilization is usually achieved with a vasectomy. In this surgery, the vas deferens from each testis is clamped, cut, or otherwise sealed (see Figure 18.11.8). This prevents sperm from traveling from the epididymis to the ejaculatory ducts and being ejaculated from the penis. The same amount of semen will still be ejaculated, but it will not contain any sperm, making fertilization impossible. After a vasectomy, the testes continue to produce sperm, but the sperm are reabsorbed. It usually takes several months after a vasectomy for all remaining sperm to be ejaculated or reabsorbed. In the meantime, another method of birth control should be used.
Female Sterilization
The procedure undertaken for female sterilization is usually tubal ligation. The oviducts may be tied or cut in a surgical procedure, which permanently blocks the tubes. Alternatively, tiny metal implants may be inserted into the oviducts in a nonsurgical procedure. Over time, scar tissue grows around the implants and permanently blocks the tubes. Either method stops eggs from traveling from the ovaries through the oviducts, where fertilization usually takes place.
Emergency Contraception
Emergency contraception is any form of contraception that is used after unprotected vaginal intercourse. One method is the so-called “morning-after” pill. This is essentially a high-dose birth control pill that helps prevent pregnancy by temporarily preventing ovulation. It works only if ovulation has not already occurred, and when taken within five days after unprotected sex. The sooner the pill is taken, the more likely it is to work. Another method of emergency contraception is the IUD. An IUD that is inserted up to five days after unprotected sex can prevent nearly 100% of pregnancies. It keeps sperm from reaching and fertilizing an egg, or inhibits implantation if an ovum has already been fertilized. The IUD can then be left in place to prevent future pregnancies.
18.11 Summary
- More than half of all fertile couples worldwide use contraception (birth control), which is any method or device used to prevent pregnancy. Different methods of contraception vary in their effectiveness, typically expressed as the failure rate, or the percentage of women who become pregnant using a given method during the first year of use. For most methods, the failure rate with typical use is much higher than the failure rate with perfect use.
- Types of birth control methods include barrier methods, hormonal methods, intrauterine devices, behavioural methods, and sterilization. Except for sterilization, all of the methods are reversible. All of the methods have health risks, but they are less than the risks of pregnancy.
- Barrier methods are devices that block sperm from entering the uterus. They include condoms and diaphragms. Of all birth control methods, only condoms can prevent the spread of sexually transmitted infections in addition to pregnancy.
- Hormonal methods involve the administration of hormones to prevent ovulation. Hormones can be administered in various ways, such as in an injection, through a skin patch, or — most commonly — in birth control pills. There are two types of birth control pills: those that contain estrogen and progesterone, and those that contain only progesterone. Both types are equally effective, but they have different potential side effects.
- An intrauterine device (IUD) is a small T-shaped plastic structure containing copper or a hormone that is inserted into the uterus by a physician and left in place for months or even years. It is highly effective even with typical use, but it does have some risks, such as increased menstrual bleeding and, rarely, perforation of the uterus.
- Behavioural methods involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present. In fertility awareness methods, unprotected intercourse is avoided during the most fertile days of the cycle, as estimated by basal body temperature or the characteristics of cervical mucus. In withdrawal (coitus interruptus), the penis is withdrawn from the vagina before ejaculation occurs. Behavioural methods are the least effective methods of contraception.
- Sterilization is the most effective contraceptive method, but it requires a surgical procedure and may be irreversible. Male sterility is usually achieved with a vasectomy, in which the vas deferens are clamped or cut to prevent sperm from being ejaculated in semen. Female sterility is usually achieved with a tubal ligation, in which the oviducts are clamped or cut to prevent sperm from reaching and fertilizing eggs.
- Emergency contraception is any form of contraception used after unprotected vaginal intercourse. One method is the “morning after” pill, which is a high-dose birth control pill that can be taken up to five days after unprotected sex. Another method is an IUD, which can be inserted up to five days after unprotected sex.
18.11 Review Questions
-
- How is the effectiveness of contraceptive methods typically measured?
- What is an IUD?
- Discuss sterilization as a birth control method. Compare sterilization in males and females.
- What is emergency contraception? When is it used? What are two forms of emergency contraception?
- How does the thickness of cervical mucus relate to fertility? How do two methods of contraception take advantage of this relationship?
- If a newly developed method of contraception had a 35% failure rate, would you consider this to be an effective method? Explain your answer.
18.11 Explore More
How do contraceptives work? – NWHunter, TED-Ed, 2016.
The History Of Birth Control | TIME, 2015.
Finally, A Male Pill? SciShow, 2012.
Attributions
Figure 18.11.1
512px-Marie_Stopes [cropped] by AdamBMorgan on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain). (Original by Unknown author: File:Marie Stopes in her laboratory, 1904.jpg).
Figure 18.11.2
Effectivenessofcontraceptives by Center for Disease Control and Prevention on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 18.11.3
Condom by Marco Verch Professional Photographer on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 18.11.4
Female condom by Ceridwen on Wikimedia Commons is used under a CC BY-SA 2.0 FR (https://creativecommons.org/licenses/by-sa/2.0/fr/deed.en) license.
Figure 18.11.5
Contraceptive_diaphragm by Axefan2 on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain).
Figure 18.11.6
1024px-Blausen_0585_IUD by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 18.11.7
Basal_Body_Temperature by BruceBlaus on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.11.8
1024px-Open_Vasectomy_ by Timdwilliamson on Wikimedia Commons is used under a CC BY SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
References
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
SciShow. (2012, August 16). Finally, a male pill? YouTube. https://www.youtube.com/watch?v=vIaL5QiKbWI&feature=youtu.be
Stopes, M. (1918). Married love. Wikisource. https://en.wikisource.org/w/index.php?title=Married_Love&oldid=6230157 (Originally published with Preface and Notes by William J. Robinson, by The Critic and Guide Company. This book was banned in the United States until 1933.)
TED-Ed. (2016, September). How do contraceptives work? – NWHunter. YouTube. https://www.youtube.com/watch?v=Zx8zbTMTncs&feature=youtu.be
Time. (2015, January 30). The history of birth control | TIME. YouTube. https://www.youtube.com/watch?v=jdr1yDO7MoY&feature=youtu.be
Wikipedia contributors. (2020, August 9). Marie Stopes. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Marie_Stopes&oldid=972063381
Any method or device used to prevent pregnancy; also called birth control.
A type of contraception in which a device such as a condom or diaphragm is used to physically block sperm from entering the uterus.
The male reproductive cell.
The female reproductive organ in which first an embryo and then a fetus grows and develops until birth.
A thin rubber sheath worn on a man's penis during sexual intercourse as a contraceptive or as a protection against infection.
A barrier method of birth control. It is a dome-shaped piece of silicon placed over the cervix with spermicide before sex and left in place for at least six hours after sex. Fitting by a healthcare provider is generally required.
The physical activity of sex between two people.
The neck of the uterus that protrudes down into the vagina and through which a canal connects the vagina and uterus.
A method of birth control which makes use of hormones such as estrogen and/or progesterone to prevent pregnancy by interfering with ovulation.
A T-shaped contraceptive structure containing copper, or a hormone that is inserted into the uterus by a physician and may be left in place for months or years.
The practice of refraining from some or all aspects of sexual activity.
The process in males in which muscle contractions propel sperm from the epididymes and out through the urethra in semen.
Surgical procedure that is generally irreversible, and makes it impossible for a woman to become pregnant or for a man to ejaculate viable, motile sperm.
Surgical sterilization procedure in males in which the vas deferens are blocked so sperm cannot be ejaculated.
One of a pair of thin tubes that transports sperm from an epididymis to an ejaculatory duct during ejaculation; also called sperm duct.
Two male reproductive organs that produce sperm and secrete testosterone; male gonad.
One of two male reproductive organs where sperm mature and are stored until they leave the body during ejaculation.
One of two tubes in the male reproductive system that joins the vas deferens with the urethra and carries semen during ejaculation.
Fluid containing sperm and glandular secretions, which nourishes sperm and carries them through the urethra and out of the body.
Surgical sterilization procedure in females in which the Fallopian tubes are blocked so sperm cannot reach and fertilize an egg.
Any form of birth control that is used after unprotected vaginal intercourse.
The release of a secondary oocyte from an ovary about half way through the menstrual cycle.
A hormone is a signaling molecule produced by glands in multicellular organisms that target distant organs to regulate physiology and behavior.

