163 18.12 Case Study Conclusion: Trying to Conceive
Created by CK-12 Foundation/Adapted by Christine Miller

Case Study Conclusion: Trying to Conceive
The woman in Figure 18.12.1 is holding a home pregnancy test. The two pink lines in the middle are the type of result that Alicia and Victor are desperately hoping to see themselves one day — a positive pregnancy test. In the beginning of the chapter you learned that Alicia and Victor have been actively trying to get pregnant for a year, which, as you now know, is the time frame necessary for infertility to be diagnosed.
Alicia and Victor tried having sexual intercourse on day 14 of her menstrual cycle to optimize their chances of having his sperm meet her ovum. Why might this not be successful, even if they do not have fertility problems? Although the average menstrual cycle is 28 days, with ovulation occurring around day 14, many women vary widely from these averages (either consistently or variably) from month to month. Recall, for example, that menstrual cycles may vary from 21 to 45 days in length, and a woman’s cycle is considered to be regular if it varies within as many as eight days from shortest to longest cycle. This variability means that ovulation often does not occur on or around day 14, particularly if the woman has significantly shorter, longer, or irregular cycles — like Alicia does. Therefore, by aiming for day 14 without knowing when Alicia is actually ovulating, they may not be successful in helping Victor’s sperm encounter Alicia’s egg.
Lack of ovulation entirely can also cause variability in menstrual cycle length. As you have learned, the regulation of the menstrual cycle depends on an interplay of hormones from the pituitary gland and ovaries, including FSH and LH from the pituitary and estrogen and progesterone from the ovary — specifically from the follicle which surrounds the maturing egg and becomes the corpus luteum after ovulation. Shifts in these hormones and processes can affect ovulation and menstrual cycle length. This is why Alicia was concerned about her long and irregular menstrual cycles. If they are a sign that she is not ovulating, that could be the reason why she is having trouble getting pregnant.
In order to get a better idea of whether Alicia is ovulating, Dr. Bashir recommended that she take her basal body temperature (BBT) each morning before getting out of bed, and track it throughout her menstrual cycle. As you have learned, BBT typically rises slightly and stays high after ovulation. While tracking BBT is not a particularly effective form of contraception, since the temperature rise occurs only after ovulation, it can be a good way to see whether a woman is ovulating at all. Although not every woman will see a clear shift in BBT after ovulation, it is a relatively easy way to start assessing a woman’s fertility and is used as part of a more comprehensive fertility assessment by some physicians.
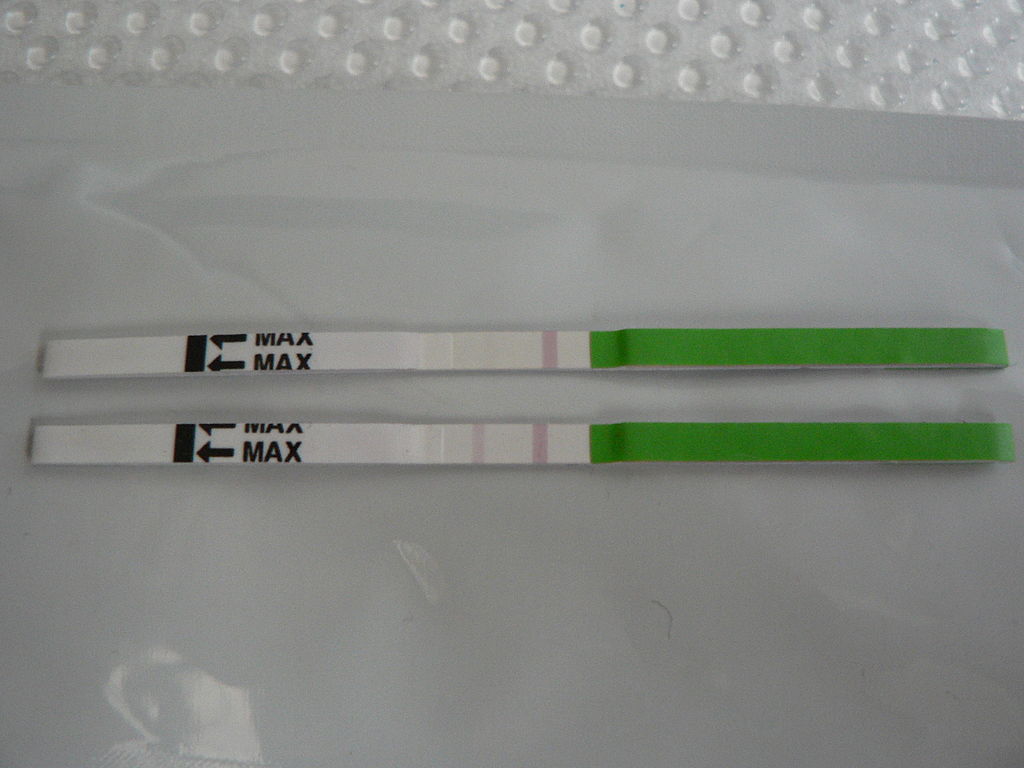
Dr. Bashir also recommended that Alicia use a home ovulation predictor kit. This is another relatively cheap and easy way to assess ovulation. Most ovulation predictor kits work by detecting the hormone LH in urine using test strips, like the ones shown in Figure 18.12.2. Why can this predict ovulation? Think about what you have learned about how ovulation is triggered. Rising levels of estrogen from the maturing follicle in the ovary causes a surge in the level of LH secreted from the pituitary gland, which triggers ovulation. This surge in LH can be detected by the home kit, which compares the level of LH in a woman’s urine to that of a control on the strip. After the LH surge is detected, ovulation will typically occur within one to two days.
By tracking her BBT and using the ovulation predictor kit, Alicia has learned that she is most likely ovulating, but not in every cycle, and sometimes she ovulates much later than day 14. Because frequent anovulatory cycles can be a sign of an underlying hormonal disorder, such as polycystic ovary syndrome (PCOS) or problems with the pituitary or other glands that regulate the reproductive system, Dr. Bashir orders blood tests for Alicia and sets up an appointment for a physical exam.
However, because Alicia is sometimes ovulating, the problem may not lie solely with her. Recall that infertility occurs in similar proportions in men and women, and can be due to problems in both partners. This is why it is generally recommended that both partners get assessed for fertility issues when they are having trouble getting pregnant after a year of trying.
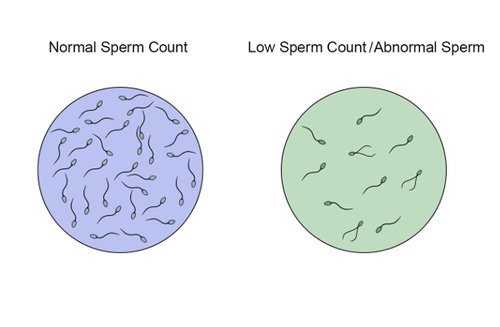
Therefore, Victor proceeds with the semen analysis that Dr. Bashir recommended. In this process, the man provides a semen sample by ejaculating into a cup or special condom, and the semen is then examined under a microscope. The semen is then checked for sperm number, shape, and motility. Sperm with an abnormal shape or trouble moving will likely have trouble reaching and fertilizing an egg. A low number of sperm will also reduce the chances of conception. In this way, semen analysis can provide insight into the possible underlying causes of infertility. For instance, a low sperm count could indicate problems in sperm production or a blockage in the male reproductive tract that is preventing sperm from being emitted from the penis. Further testing would have to be done to distinguish between these two possible causes.
Victor had been worried that past injuries to his testes may have affected his fertility. You may remember the testes are where sperm are produced, and because they are external to the body, they are vulnerable to injury. In addition to physical damage to the testes and other parts of the male reproductive tract, a testicular injury could potentially cause the creation of antibodies against a man’s own sperm. As you have learned, Sertoli cells lining the seminiferous tubules are tightly packed so that the developing sperm are normally well-separated from the body’s immune system. However, in the case of an injury, this barrier can be breached, which can cause the creation of antisperm antibodies. These antibodies can hamper fertility by killing the sperm, or otherwise interfering with their ability to move or fertilize an egg. When infertility is due to such antibodies, it is called “immune infertility.”
Victor’s semen analysis shows that he has normal numbers of healthy sperm. Dr. Bashir recommends that while they investigate whether Alicia has an underlying medical issue, she continue to track her BBT and use ovulation predictor kits to try to pinpoint when she is ovulating. She recommends that once Alicia sees an LH surge, the couple try to have intercourse within three days to maximize their chances of conception. If Alicia is found to have a medical problem that is inhibiting ovulation, depending on what it is, they may either address the problem directly, or she can take medication that stimulates ovulation, such as clomiphene citrate (often sold under the brand name Clomid). This medication works by increasing the amount of FSH secreted by the pituitary.
Fortunately, tracking ovulation at home and timing intercourse appropriately was all Alicia and Victor needed to do to finally get pregnant! After their experience, they, like you, now have a much deeper understanding of the intricacies of the reproductive system and the complex biology that is involved in the making of a new human organism.
Chapter 18 Summary
In this chapter, you learned about the male and female reproductive systems. Specifically, you learned that:
- The reproductive system is the human organ system responsible for the production and fertilization of gametes and, in females, the carrying of a fetus.
- Both male and female reproductive systems have organs called gonads (testes in males, ovaries in females) that produce gametes (sperm or ova) and sex hormones (such as testosterone in males and estrogen in females). Sex hormones are endocrine hormones that control prenatal development of sex organs, sexual maturation at puberty, and reproduction after puberty.
- The reproductive system is the only organ system that is significantly different between males and females. A Y-chromosome gene called SRY is responsible for undifferentiated embryonic tissues developing into a male reproductive system. Without a Y chromosome, the undifferentiated embryonic tissues develop into a female reproductive system.
- Male and female reproductive systems are different at birth, but immature and nonfunctioning. Maturation of the reproductive system occurs during puberty when hormones from the hypothalamus and pituitary gland stimulate the gonads to produce sex hormones again. The sex hormones, in turn, cause the physical changes experienced during puberty.
- Male reproductive system organs include the testes, epididymis, penis, vas deferens, prostate gland, and seminal vesicles.
-
- The two testes are sperm- and testosterone-producing male gonads. They are contained within the scrotum, a pouch that hangs down behind the penis. The testes are filled with hundreds of tiny, tightly coiled seminiferous tubules, where sperm are produced. The tubules contain sperm in different stages of development, as well as Sertoli cells, which secrete substances needed for sperm production. Between the tubules are Leydig cells, which secrete testosterone.
- The two epididymides are contained within the scrotum. Each epididymis is a tightly coiled tubule where sperm mature and are stored until they leave the body during an ejaculation.
- The two vas deferens are long, thin tubes that run from the scrotum up into the pelvic cavity. During ejaculation, each vas deferens carries sperm from one of the epididymides to one of the pair of ejaculatory ducts.
- The two seminal vesicles are glands within the pelvis that secrete fluid through ducts into the junction of each vas deferens and ejaculatory duct. This alkaline fluid makes up about 70% of semen, the sperm-containing fluid that leaves the penis during ejaculation. Semen contains substances and nutrients that sperm need to survive and “swim” in the female reproductive tract.
- The prostate gland is located just below the seminal vesicles and surrounds the urethra and its junction with the ejaculatory ducts. The prostate secretes an alkaline fluid that makes up close to 30% of semen. Prostate fluid contains a high concentration of zinc, which sperm need to be healthy and motile.
- The ejaculatory ducts form where the vas deferens joins with the ducts of the seminal vesicles in the prostate gland. They connect the vas deferens with the urethra. The ejaculatory ducts carry sperm from the vas deferens, and secretions from the seminal vesicles and prostate gland that together form semen.
- The paired bulbourethral glands are located just below the prostate gland. They secrete a tiny amount of fluid into semen. The secretions help lubricate the urethra and neutralize any acidic urine it may contain.
- The penis is the external male organ that has the reproductive function of intromission, which is delivering sperm to the female reproductive tract. The penis also serves as the organ that excretes urine. The urethra passes through the penis and carries urine or semen out of the body. Internally, the penis consists largely of columns of spongy tissue that can fill with blood and make the penis stiff and erect. This is necessary for sexual intercourse so intromission can occur.
- Parts of a mature sperm include the head, acrosome, midpiece, and flagellum. The process of producing sperm is called spermatogenesis. This normally starts during puberty and continues uninterrupted until death.
-
- Spermatogenesis occurs in the seminiferous tubules in the testes, and requires high concentrations of testosterone. Sertoli cells in the testes play many roles in spermatogenesis, including concentrating testosterone under the influence of follicle stimulating hormone (FSH) from the pituitary gland.
- Spermatogenesis begins with a diploid stem cell called a spermatogonium, which undergoes mitosis to produce a primary spermatocyte. The primary spermatocyte undergoes meiosis I to produce haploid secondary spermatocytes, and these cells in turn, undergo meiosis II to produce spermatids. After the spermatids grow a tail and undergo other changes, they become sperm.
- Before sperm are able to “swim,” they must mature in the epididymis. The mature sperm are then stored in the epididymis until ejaculation occurs.
- Ejaculation is the process in which semen is propelled by peristalsis in the vas deferens and ejaculatory ducts from the urethra in the penis.
- Leydig cells in the testes secrete testosterone under the control of luteinizing hormone (LH) from the pituitary gland. Testosterone is needed for male sexual development at puberty and to maintain normal spermatogenesis after puberty. It also plays a role in prostate function and the ability of the penis to become erect.
- Disorders of the male reproductive system include erectile dysfunction (ED), epididymitis, prostate cancer, and testicular cancer.
-
- ED is a disorder characterized by the regular and repeated inability of a sexually mature male to obtain and maintain an erection. ED is a common disorder that occurs when normal blood flow to the penis is disturbed or there are problems with the nervous control of penile engorgement or arousal.
-
-
- Possible physiological causes of ED include aging, illness, drug use, tobacco smoking, and obesity, among others. Possible psychological causes of ED include stress, performance anxiety, and mental disorders.
- Treatments for ED may include lifestyle changes, such as stopping smoking and adopting a healthier diet and regular exercise. However, the first-line treatment is prescription drugs such as Viagra® or Cialis® that increase blood flow to the penis. Vacuum pumps or penile implants may be used to treat ED if other types of treatment fail.
- Epididymitis is inflammation of the epididymis. It is a common disorder, especially in young men. It may be acute or chronic and is often caused by a bacterial infection. Treatments may include antibiotics, anti-inflammatory drugs, and painkillers. Treatment is important to prevent the possible spread of infection, permanent damage to the epididymis or testes, and even infertility.
- Prostate cancer is the most common type of cancer in men and the second leading cause of cancer death in men. If there are symptoms, they typically involve urination, such as frequent or painful urination. Risk factors for prostate cancer include older age, family history, a high-meat diet, and sedentary lifestyle, among others.
-
-
-
- Prostate cancer may be detected by a physical exam or a high level of prostate-specific antigen (PSA) in the blood, but a biopsy is required for a definitive diagnosis. Prostate cancer is typically diagnosed relatively late in life, and is usually slow growing, so no treatment may be necessary. In younger patients or those with faster-growing tumors, treatment is likely to include surgery to remove the prostate, followed by chemotherapy and/or radiation therapy.
- Testicular cancer, or cancer of the testes, is the most common cancer in males between the ages of 20 and 39 years. It is more common in males of European than African ancestry. A lump or swelling in one testis, fluid in the scrotum, and testicular pain or tenderness are possible signs and symptoms of testicular cancer.
-
-
-
- Testicular cancer can be diagnosed by a physical exam and diagnostic tests, such as ultrasound or blood tests. Testicular cancer has one of the highest cure rates of all cancers. It is typically treated with surgery to remove the affected testis, and this may be followed by radiation therapy, and/or chemotherapy. Normal male reproductive functions are still possible after one testis is removed, if the remaining testis is healthy.
-
- The female reproductive system is made up of internal and external organs that function to produce haploid female gametes called ova, secrete female sex hormones (such as estrogen), and carry and give birth to a fetus.
- Female reproductive system organs include the ovaries, oviducts, uterus, vagina, clitoris, and labia.
-
- The vagina is an elastic, muscular canal that can accommodate the penis. It is where sperm are usually ejaculated during sexual intercourse. The vagina is also the birth canal, and it channels the flow of menstrual blood from the uterus. A healthy vagina has a balance of symbiotic bacteria and an acidic pH.
- The uterus is a muscular organ above the vagina where a fetus develops. Its muscular walls contract to push out the fetus during childbirth. The cervix is the neck of the uterus that extends down into the vagina. It contains a canal connecting the vagina and uterus for sperm or an infant to pass through. The innermost layer of the uterus, the endometrium, thickens each month in preparation for an embryo but is shed in the following menstrual period if fertilization does not occur.
- The oviducts extend from the uterus to the ovaries. Waving fimbriae at the ovary ends of the oviducts guide ovulated ova into the tubes where fertilization may occur as the ova travel to the uterus. Cilia and peristalsis help eggs move through the tubes. Tubular fluid helps nourish sperm as they swim up the tubes toward eggs.
- The ovaries are gonads that produce eggs and secrete sex hormones including estrogen. Nests of cells called follicles in the ovarian cortex are the functional units of ovaries. Each follicle surrounds an immature ovum. At birth, a baby girl’s ovaries contain at least a million eggs, and they will not produce any more during her lifetime. One egg matures and is typically ovulated each month during a woman’s reproductive years.
- The vulva is a general term for external female reproductive organs. The vulva includes the clitoris, two pairs of labia, and openings for the urethra and vagina. Secretions from Bartholin’s glands near the vaginal opening lubricate the vulva.
- The breasts are technically not reproductive organs, but their mammary glands produce milk to feed an infant after birth. Milk drains through ducts and sacs and out through the nipple when a baby sucks.
- Oogenesis is the process of producing eggs in the ovaries of a female fetus. Oogenesis begins when a diploid oogonium divides by mitosis to produce a diploid primary oocyte. The primary oocyte begins meiosis I and then remains at this stage in an immature ovarian follicle until after birth.
- After puberty, one follicle a month matures and its primary oocyte completes meiosis I to produce a secondary oocyte, which begins meiosis II. During ovulation, the mature follicle bursts open and the secondary oocyte leaves the ovary and enters a oviducts.
- While a follicle is maturing in an ovary each month, the endometrium in the uterus is building up to prepare for an embryo. Around the time of ovulation, cervical mucus becomes thinner and more alkaline to help sperm reach the secondary oocyte.
- If the secondary oocyte is fertilized by a sperm, it quickly completes meiosis II and forms a diploid zygote, which will continue through the oviducts. The zygote will go through multiple cell divisions before reaching and implanting in the uterus. If the secondary oocyte is not fertilized, it will not complete meiosis II, and will soon disintegrate.
- Pregnancy is the carrying of one or more offspring from fertilization until birth. The maternal organism must provide all the nutrients and other substances needed by the developing offspring, and also remove its wastes. She should also avoid exposures that could potentially damage the offspring, especially early in the pregnancy when organ systems are developing.
-
- The average duration of pregnancy is 40 weeks (from the first day of the last menstrual period) and is divided into three trimesters of about three months each. Each trimester is associated with certain events and conditions that a pregnant woman may expect, such as morning sickness during the first trimester, feeling fetal movements for the first time during the second trimester, and rapid weight gain in both fetus and mother during the third trimester.
- Labour, which is the general term for the birth process, usually begins around the time the amniotic sac breaks and its fluid leaks out. Labour occurs in three stages: dilation of the cervix, birth of the baby, and delivery of the placenta (afterbirth).
- The physiological function of female breasts is lactation, or the production of breast milk to feed an infant. Sucking on the breast by the infant stimulates the release of the hypothalamic hormone oxytocin from the posterior pituitary, which causes the flow of milk. The release of milk stimulates the baby to continue sucking, which in turn keeps the milk flowing. This is one of the few examples of positive feedback in the human organism.
- The ovaries produce female sex hormones, including estrogen and progesterone. Estrogen is responsible for sexual maturation and secondary sex characteristics at puberty. It is also needed to help regulate the menstrual cycle and ovulation after puberty until menopause. Progesterone prepares the uterus for pregnancy each month during the menstrual cycle, and helps maintain the pregnancy if fertilization occurs.
- The menstrual cycle refers to natural changes that occur in the female reproductive system each month during the reproductive years, except when a woman is pregnant. The cycle is necessary for the production of ova and the preparation of the uterus for pregnancy. It involves changes in both the ovaries and uterus and is controlled by pituitary hormones (FSH and LH) and ovarian hormones (estrogen and progesterone).
-
- The female reproductive period is delineated by menarche, or the first menstrual period, which usually occurs around age 12 or 13; and by menopause, or the cessation of menstrual periods, which typically occurs around age 52. A typical menstrual cycle averages 28 days in length but may vary normally from 21 to 45 days. The average menstrual period is five days long, but may vary normally from two to seven days. These variations in the menstrual cycle may occur both between women and within individual women from month to month.
- The events of the menstrual cycle that take place in the ovaries make up the ovarian cycle. It includes the follicular phase, when a follicle and its ovum mature due to rising levels of FSH; ovulation, when the ovum is released from the ovary due to a rise in estrogen and a surge in LH; and the luteal phase, when the follicle is transformed into a structure called a corpus luteum that secretes progesterone. In a 28-day menstrual cycle, the follicular and luteal phases typically average about two weeks in length, with ovulation generally occurring around day 14 of the cycle.
- The events of the menstrual cycle that take place in the uterus make up the uterine cycle. It includes menstruation, which generally occurs on days 1 to 5 of the cycle and involves shedding of endometrial tissue that built up during the preceding cycle; the proliferative phase, during which the endometrium builds up again until ovulation occurs; and the secretory phase, which follows ovulation and during which the endometrium secretes substances and undergoes other changes that prepare it to receive an embryo.
- Disorders of the female reproductive system include cervical cancer, vaginitis, and endometriosis.
-
- Cervical cancer occurs when cells of the cervix grow abnormally and develop the ability to invade nearby tissues, or spread to other parts of the body. Worldwide, cervical cancer is the second-most common type of cancer in females and the fourth-most common cause of cancer death in females. Early on, cervical cancer often has no symptoms; later, symptoms such as abnormal vaginal bleeding and pain are likely.
-
-
- Most cases of cervical cancer occur because of infection with human papillomavirus (HPV), so the HPV vaccine is expected to greatly reduce the incidence of the disease. Other risk factors include smoking and a weakened immune system. A Pap smear can diagnose cervical cancer at an early stage. Where Pap smears are done routinely, cervical cancer death rates have fallen dramatically. Treatment of cervical cancer generally includes surgery, which may be followed by radiation therapy or chemotherapy.
- Vaginitis is inflammation of the vagina. A discharge is likely, and there may be itching and pain. About 90% of cases of vaginitis are caused by infection with microorganisms, typically by the yeast Candida albicans. A minority of cases are caused by irritants or allergens in products such as soaps, spermicides, or douches.
-
-
-
- Diagnosis of vaginitis may be based on characteristics of the discharge, which can be examined microscopically or cultured. Treatment of vaginitis depends on the cause, and is usually an oral or topical anti-fungal or antibiotic medication.
- Endometriosis is a disease in which endometrial tissue grows outside the uterus. This tissue may bleed during the menstrual period and cause inflammation, pain, and scarring. The main symptom of endometriosis is pelvic pain, which may be severe. Endometriosis may also lead to infertility.
-
-
-
- Endometriosis is thought to have multiple causes, including genetic mutations. Retrograde menstruation may be the immediate cause of endometrial tissue escaping the uterus and entering the pelvic cavity. Endometriosis is usually treated with surgery to remove the abnormal tissue and medication for pain. If surgery is more conservative than hysterectomy, endometriosis may recur.
-
- Infertility is the inability of a sexually mature adult to reproduce by natural means. It is defined scientifically and medically as the failure to achieve a successful pregnancy after at least one year of regular, unprotected sexual intercourse.
- About 40% of infertility in couples is due to female infertility, and another 30% is due to male infertility. In the remaining cases, a couple’s infertility is due to problems in both partners or to unknown causes.
- Male infertility occurs when there are no or too few healthy, motile sperm. This may be caused by problems with spermatogenesis or by blockage of the male reproductive tract that prevents sperm from being ejaculated. Risk factors for male infertility include heavy alcohol use, smoking, certain medications, and advancing age, to name just a few.
- Female infertility occurs due to failure to produce viable ova by the ovaries or structural problems in the oviducts or uterus. Polycystic ovary syndrome is the most common cause of failure to produce viable eggs. Endometriosis and uterine fibroids are possible causes of structural problems in the oviducts and uterus. Risk factors for female infertility include smoking, stress, poor diet, and older age, among others.
- Diagnosing the cause(s) of a couple’s infertility generally requires testing both the man and the woman for potential problems. For men, semen is likely to be examined for adequate numbers of healthy, motile sperm. For women, signs of ovulation are monitored, for example, with an ovulation test kit or ultrasound of the ovaries. For both partners, the reproductive tract may be medically imaged to look for blockages or other abnormalities.
-
- Treatments for infertility depend on the cause. For example, if a medical problem is interfering with sperm production, medication may resolve the underlying problem so sperm production is restored. Blockages in either the male or the female reproductive tract can often be treated surgically. If there are problems with ovulation, hormonal treatments may stimulate ovulation.
- Some cases of infertility are treated with assisted reproductive technology (ART). This is a collection of medical procedures in which eggs and sperm are taken from the couple and manipulated in a lab to increase the chances of fertilization occurring and an embryo forming. Other approaches for certain causes of infertility include the use of a surrogate mother, gestational carrier, or sperm donation.
- Infertility can negatively impact a couple socially and psychologically, and it may be a major cause of marital friction or even divorce. Infertility treatments may raise ethical issues relating to the costs of the procedures and the status of embryos that are created in vitro but not used for pregnancy. Infertility is an under-appreciated problem in developing countries where birth rates are high and children have high economic as well as social value. In these countries, poor health care is likely to lead to more problems with infertility and fewer options for treatment.
- More than half of all fertile couples worldwide use contraception (birth control), which is any method or device used to prevent pregnancy. Different methods of contraception vary in their effectiveness, typically expressed as the failure rate, or the percentage of women who become pregnant using a given method during the first year of use. For most methods, the failure rate with typical use is much higher than the failure rate with perfect use.
- Types of birth control methods include barrier methods, hormonal methods, intrauterine devices, behavioural methods, and sterilization. Except for sterilization, all of the methods are reversible.
-
- Barrier methods are devices that block sperm from entering the uterus. They include condoms and diaphragms. Of all birth control methods, only condoms can also prevent the spread of sexually transmitted infections.
- Hormonal methods involve the administration of hormones to prevent ovulation. Hormones can be administered in various ways, such as in an injection, through a skin patch, or, most commonly, in birth control pills. There are two types of birth control pills: those that contain estrogen and progesterone, and those that contain only progesterone. Both types are equally effective, but they have different potential side effects.
- An intrauterine device (IUD) is a small T-shaped plastic structure containing copper or a hormone that is inserted into the uterus by a physician and left in place for months or even years. It is highly effective even with typical use, but it does have some risks, such as increased menstrual bleeding and, rarely, perforation of the uterus.
- Behavioural methods involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present. In fertility awareness methods, unprotected intercourse is avoided during the most fertile days of the cycle as estimated by basal body temperature or the characteristics of cervical mucus. In withdrawal, the penis is withdrawn from the vagina before ejaculation occurs. Behavioural methods are the least effective methods of contraception.
- Sterilization is the most effective contraceptive method, but it requires a surgical procedure and may be irreversible. Male sterility is usually achieved with a vasectomy, in which the vas deferens are clamped or cut to prevent sperm from being ejaculated in semen. Female sterility is usually achieved with a tubal ligation, in which the oviducts are clamped or cut to prevent sperm from reaching and fertilizing eggs.
- Emergency contraception is any form of contraception that is used after unprotected vaginal intercourse. One method is the “morning after” pill, which is a high-dose birth control pill that can be taken up to five days after unprotected sex. Another method is an IUD, which can be inserted up to five days after unprotected sex.
In this chapter, you learned how the male and female reproductive systems work together to produce a zygote. In the next chapter, you will learn about how the human organism grows and develops throughout life — from a zygote all the way through old age.
Chapter 18 Review
-
- Which glands produce the non-sperm fluids that make up semen? What is the rough percentage of each fluid in semen?
- What is one reason why semen’s alkalinity assists in reproduction?
- What are three things that pass through the cervical canal of females, going in either direction?
- Other than where the cancer originates, what is one difference between prostate and testicular cancer?
- If a woman is checking her basal body temperature each morning as a form of contraception, and today is day 12 of her menstrual cycle and her basal body temperature is still low, is it safe for her to have unprotected sexual intercourse today? Why or why not?
-
- Where is a diaphragm placed? How does it work to prevent pregnancy?
- Why are the testes located outside of the body?
- Why is it important to properly diagnose the causative agent when a woman has vaginitis?
- Describe two ways in which sperm can move through the male and/or female reproductive tracts.
Attributions
Figure 18.12.1
Pregnancy test/ Dos rayitas by Esparta Palma on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 18.12.2
1024px-Ovulatietest by Sapp on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 18.12.3
Sperm Count by CK-12 Foundation is used under a CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
References
Brainard, J/ CK-12 Foundation. (2016). Figure 3 Normal vs. low sperm count [digital image]. In CK-12 College Human Biology (Section 20.12) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-college-human-biology/section/20.12/
The physical activity of sex between two people.
The monthly cycle of processes and events in the ovaries and uterus of a sexually mature human female until menopause.
The male reproductive cell.
The gamete produced by a female.
The release of a secondary oocyte from an ovary about half way through the menstrual cycle.
A hormone is a signaling molecule produced by glands in multicellular organisms that target distant organs to regulate physiology and behavior.
The master gland of the endocrine system that secretes many hormones, the majority of which regulate other endocrine glands.
A pair of female reproductive organs that produces eggs and secretes estrogen.
A hormone secreted by the anterior pituitary gland which promotes the formation of ova or sperm.
A hormone secreted by the anterior pituitary gland that stimulates ovulation in females and the synthesis of androgen in males.
The female sex hormone secreted mainly by the ovaries.
The female sex hormone secreted mainly by the ovaries that helps maintain a successful pregnancy.
The functional unit of an ovary that consists of a nest of epithelial cells surrounding an egg.
An ovarian structure that forms from a follicle after it matures and ovulates an egg.
Fluid containing sperm and glandular secretions, which nourishes sperm and carries them through the urethra and out of the body.
A type of cell that lines the seminiferous tubules in the testes and plays several roles in sperm production.
One of the many tiny tubes contained within the testes where sperm are produced.
The fusion of haploid gametes, egg and sperm, to form the diploid zygote.
A mature haploid male or female germ cell which is able to unite with another of the opposite sex in sexual reproduction to form a zygote.
An unborn offspring of a mammal, in particular an unborn human baby more than eight weeks after conception.
One of a pair of organs that secrete sex hormones and produce gametes; testis in males and ovary in females.
Two male reproductive organs that produce sperm and secrete testosterone; male gonad.
The male sex hormone secreted mainly by the testes.
A period during which humans become sexually mature.
A part of the brain that secretes hormones and connects the brain with the endocrine system.
One of two male reproductive organs where sperm mature and are stored until they leave the body during ejaculation.
The male reproductive organ containing the urethra, through which semen and urine pass out of the body.
One of a pair of thin tubes that transports sperm from an epididymis to an ejaculatory duct during ejaculation; also called sperm duct.
A gland in the male reproductive system that secretes fluid into semen and provides nourishing substances to sperm.
One of a pair of glands of the male reproductive system that secretes fluid into semen.
A pouch-like external structure of the male reproductive system, located behind the penis, that contains the testes, epididymes, and part of the vas deferens.
A type of cell found between seminiferous tubules in the testes that produces and secretes testosterone.
The process in males in which muscle contractions propel sperm from the epididymes and out through the urethra in semen.
A body cavity that is bounded by the bones of the pelvis. Its oblique roof is the pelvic inlet (the superior opening of the pelvis). Its lower boundary is the pelvic floor. The pelvic cavity primarily contains reproductive organs, the urinary bladder, the pelvic colon, and the rectum.
One of a pair of glands in the male reproductive system that secretes a fluid to help lubricate the urethra and neutralize any urine it may contain before ejaculation occurs (also called Cowper’s gland).
The process in which a male’s penis deposits sperm in a female’s vagina.
The part of the sperm that contains the nucleus.
An organelle covering the head of animal sperm and containing enzymes that digest the egg cell coating, thus permitting the sperm to enter the egg.
The central part of the sperm cell between the head and the tail.
A whip-like structure that allows a cell to move.
The production or development of mature spermatozoa.
Describes a cell that contain two copies of each chromosome.
A diploid stem cell in a testis that undergoes mitosis to begin the process of spermatogenesis.
A part of the cell cycle when replicated chromosomes are separated into two new nuclei and then subsequent cell division gives rise to genetically identical cells in which the number of chromosomes is maintained.
A distinctive pattern of smooth muscle contractions that propels foodstuffs distally through the esophagus and intestines.
A disorder characterized by the regular and repeated inability of a sexually mature male to obtain or maintain an erection of the penis.
inflammation of the epididymis, which may be acute or chronic
A tumor in the prostate gland of the male reproductive system that is the most common type of cancer in men.
Cancer of the testes, which is more common in younger men.
One of two female reproductive organs that carry eggs from an ovary to the uterus and are the site where fertilization usually takes place.
The female reproductive organ in which first an embryo and then a fetus grows and develops until birth.
The female reproductive organ that receives sperm during sexual intercourse and provides a passageway for a baby to leave the mother’s body during birth.
The small, sensitive external female organ that is part of the vulva and may lead to sexual arousal and/or orgasm when stimulated.
The “lips” of the vulva, consisting of folds of tissue that protect the urethral and vaginal openings.
Any type of a close and long-term biological interaction between two different biological organisms.
Any member of a large group of unicellular microorganisms which have cell walls but lack organelles and an organized nucleus, including some which can cause disease.
A measure of the acidity or basicity of aqueous or other liquid solutions. The term translates the values of the concentration of the hydrogen ion in a scale ranging from 0 and 14. In pure water, which is neutral (neither acidic nor alkaline), the concentration of the hydrogen ion corresponds to a pH of 7. A solution with a pH less than 7 is considered acidic; a solution with a pH greater than 7 is considered basic, or alkaline.
The neck of the uterus that protrudes down into the vagina and through which a canal connects the vagina and uterus.
The innermost layer of the uterus that builds up during each menstrual cycle and helps nourish the embryo if fertilization occurs or is shed from the uterus as menstrual flow if fertilization does not occur.
Small, fingerlike projections at the end of the oviducts, through which eggs move from the ovaries to the uterus. The fimbriae are connected to the ovary.
Tiny hairlike organelles, identical in structure to flagella, that line the surfaces of certain cells and beat in rhythmic waves, providing locomotion to ciliate protozoans and moving liquids along internal epithelial tissue in animals.
External female reproductive structures, including the clitoris, labia, and vaginal and urethral openings.
A tube-like organ of the urinary system that carries urine out of the body from the bladder and, in males, also carries semen out of the body.
Refers to the front of the chest or, more specifically, to the mammary gland. The mammary gland is a milk producing gland. It is composed largely of fat.
An exocrine gland in humans and other mammals that produces milk to feed young offspring. Mammals get their name from the Latin word mamma, "breast".
The production or development of an ovum.
A cell in an ovary which may undergo meiotic division to form an ovum.
A stage of growth and development that occurs from implantation in the uterus through the eighth week after fertilization.
The union of the sperm cell and the egg cell. Also known as a fertilized ovum, the zygote begins as a single cell but divides rapidly in the days following fertilization. After this two-week period of cell division, the zygote eventually becomes an embryo.
The carrying of one or more offspring from fertilization until birth.
A general term for the process of childbirth, which includes three stages: dilation of the cervical canal, birth of the child, and delivery of the placenta (afterbirth).
The production of breastmilk to feed an infant.
An endocrine hormone secreted by the pituitary gland that controls a variety of functions, including during childbirth to stimulate uterine contractions and during lactation to trigger milk letdown.
A control mechanism that serves to intensify a response until an endpoint is reached.
The beginning of menstruation; first monthly period in a female.
The cessation of a woman’s menstrual cycles, usually by age 52.
The series of events of the menstrual cycle that occur in the ovaries, including maturation of a follicle, ovulation, and development of the corpus luteum.
The phase of the ovarian cycle during which follicles in the ovary mature. It ends with ovulation. The main hormones controlling this stage are follicle-stimulating hormone and gonadotropin-releasing hormone.
The later phase of the ovarian cycle. It begins with the formation of the corpus luteum and ends in either pregnancy or degeneration of the corpus luteum.
The events of the menstrual cycle that occur in the uterus, including menses and the buildup of the endometrium.
The process in which the endometrium of the uterus is shed from the body during the first several days of the menstrual cycle; also called monthly period or menses.
The second phase of the uterine cycle when estrogen causes the endometrium lining of the uterus to grow, or proliferate, during this time.
The stage of the menstrual cycle immediately following ovulation, during which the womb lining is at full thickness and its mucus glands are actively secreting.
Cancer of the cervix of the uterus, usually caused by infection with human papillomavirus (HPV).
An inflammation of the vagina usually caused by an infection with microbes.
A disease in which endometrial tissue grows outside the uterus, typically causing pain and bleeding.
A sexually transmitted virus that may cause genital warts and cervical cancer.
A medical test in which cells are scraped from the cervix and examined under a microscope in order to detect cancer cells, or precancerous cells, if they are present.
An organisms that is so small it is invisible to the human eye.
The failure to achieve a successful pregnancy after at least one year of regular, unprotected sexual intercourse.
A collection of medical procedures in which eggs and sperm are removed from an infertile couple and manipulated in ways that increase the chances of fertilization occurring, such as in-vitro fertilization
A type of contraception in which a device such as a condom or diaphragm is used to physically block sperm from entering the uterus.
Surgical procedure that is generally irreversible, and makes it impossible for a woman to become pregnant or for a man to ejaculate viable, motile sperm.


