92 9.7 Pancreas
Created by CK-12 Foundation/Adapted by Christine Miller

A Shot in the Arm
Giving yourself an injection can be difficult, but for someone with diabetes, it may be a matter of life or death. The person in the photo has diabetes and is injecting themselves with insulin, the hormone that helps control the level of glucose in the blood. Insulin is produced by the pancreas.
Introduction to the Pancreas
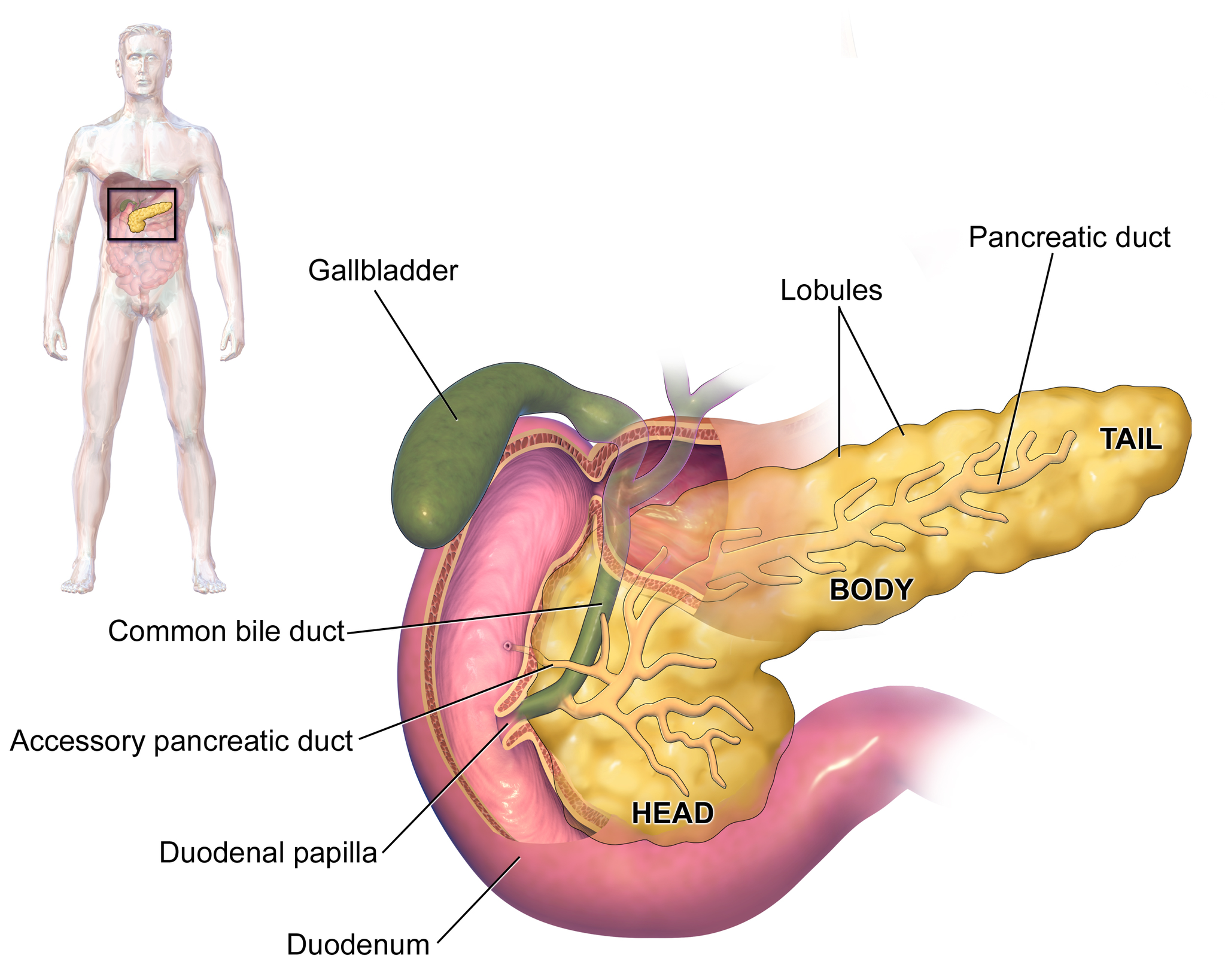
The pancreas is a large gland located in the upper left abdomen behind the stomach, as shown in Figure 9.7.2. The pancreas is about 15 cm (6 in) long, and it has a flat, oblong shape. Structurally, the pancreas is divided into a head, body, and tail. Functionally, the pancreas serves as both an endocrine gland and an exocrine gland.
- As an endocrine gland, the pancreas is part of the endocrine system. As such, it releases hormones (such as insulin) directly into the bloodstream for transport to cells throughout the body.
- As an exocrine gland, the pancreas is part of the digestive system. As such, it releases digestive enzymes into ducts that carry the enzymes to the gastrointestinal tract, where they assist with digestion. In this concept, the focus is on the pancreas as an endocrine gland. You can read about the pancreas as an exocrine gland in Chapter 15 Digestive System.
The Pancreas as an Endocrine Gland
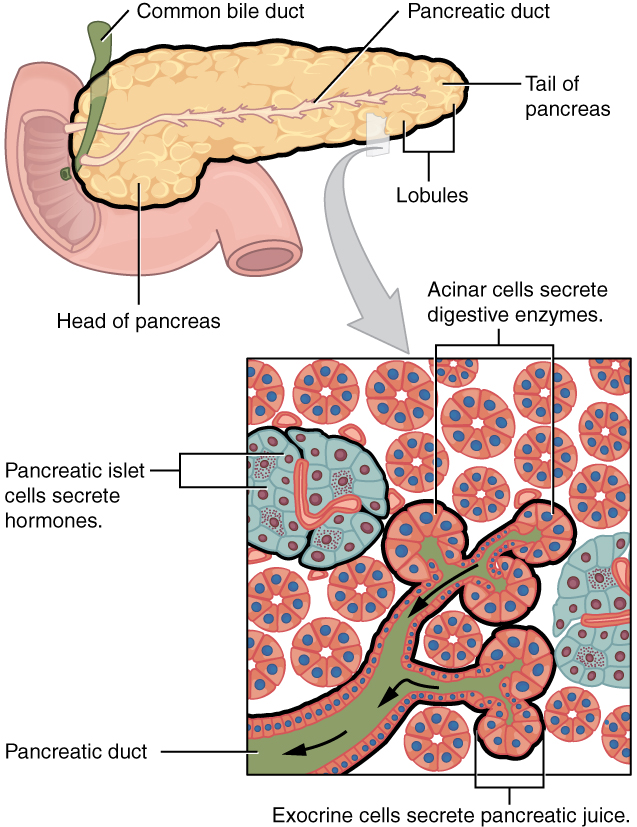
The tissues within the pancreas that have an endocrine role exist as clusters of cells called pancreatic islets. They are also called the islets of Langerhans. You can see pancreatic tissue, including islets, in Figure 9.7.3. There are approximately three million pancreatic islets, and they are crisscrossed by a dense network of capillaries. The capillaries are lined by layers of islet cells that have direct contact with the blood vessels, into which they secrete their endocrine hormones.
The pancreatic islets consist of four main types of cells, each of which secretes a different endocrine hormone. All of the hormones produced by the pancreatic islets, however, play crucial roles in glucose metabolism and the regulation of blood glucose levels, among other functions.
- Islet cells called alpha (α) cells secrete the hormone glucagon. The function of glucagon is to increase the level of glucose in the blood. It does this by stimulating the liver to convert stored glycogen into glucose, which is released into the bloodstream.
- Islets cells called beta (β) cells secrete the hormone insulin. The function of insulin is to decrease the level of glucose in the blood. It does this by promoting the absorption of glucose from the blood into fat, liver, and skeletal muscle cells. In these tissues, the absorbed glucose is converted into glycogen, fats (triglycerides), or both.
- Islet cells called delta (δ) cells secrete the hormone somatostatin. This hormone is also called growth hormone inhibiting hormone, because it inhibits the anterior lobe of the pituitary gland from producing growth hormone. Somatostatin also inhibits the secretion of pancreatic endocrine hormones and pancreatic exocrine enzymes.
- Islet cells called gamma (γ) cells secrete the hormone pancreatic polypeptide. The function of pancreatic polypeptide is to help regulate the secretion of both endocrine and exocrine substances by the pancreas.
Disorders of the Pancreas
There are a variety of disorders that affect the pancreas. They include pancreatitis, pancreatic cancer, and diabetes mellitus.
Pancreatitis

Pancreatitis is inflammation of the pancreas. It has a variety of possible causes, including gallstones, chronic alcohol use, infections (such as measles or mumps), and certain medications. Pancreatitis occurs when digestive enzymes produced by the pancreas damage the gland’s tissues, which causes problems with fat digestion. The disorder is usually associated with intense pain in the central abdomen, and the pain may radiate to the back. Yellowing of the skin and whites of the eyes (see Figure 9.7.4), which is called jaundice, is a common sign of pancreatitis. People with pancreatitis may also have pale stools and dark urine. Treatment of pancreatitis includes administering drugs to manage pain, and addressing the underlying cause of the disease, for example, by removing gallstones.
Pancreatic Cancer
There are several different types of pancreatic cancer that may affect either the endocrine or the exocrine tissues of the gland. Cancers affecting the endocrine tissues are all relatively rare. However, their incidence has been rising sharply. It is unclear to what extent this reflects increased detection, especially through medical imaging techniques. Unfortunately, pancreatic cancer is usually diagnosed at a relatively late stage when it is too late for surgery, which is the only way to cure the disorder. In 2020 it is estimated that 6,000 Canadians will be newly diagnosed with pancreatic cancer, and that during this same year, 5,300 will die of pancreatic cancer.
While it is rare before the age of 40, pancreatic cancer occurs most often after the age of 60. Factors that increase the risk of developing pancreatic cancer include smoking, obesity, diabetes, and a family history of the disease. About one in four cases of pancreatic cancer are attributable to smoking. Certain rare genetic conditions are also risk factors for pancreatic cancer.
Diabetes Mellitus
By far the most common type of pancreatic disorder is diabetes mellitus, more commonly called simply diabetes. There are many different types of diabetes, but diabetes mellitus is the most common. It occurs in two major types, type 1 diabetes and type 2 diabetes. The two types have different causes and may also have different treatments, but they generally produce the same initial symptoms, which include excessive urination and thirst. These symptoms occur because the kidneys excrete more urine in an attempt to rid the blood of excess glucose. Loss of water in urine stimulates greater thirst. Other signs and symptoms of diabetes are listed in Figure 9.7.5.
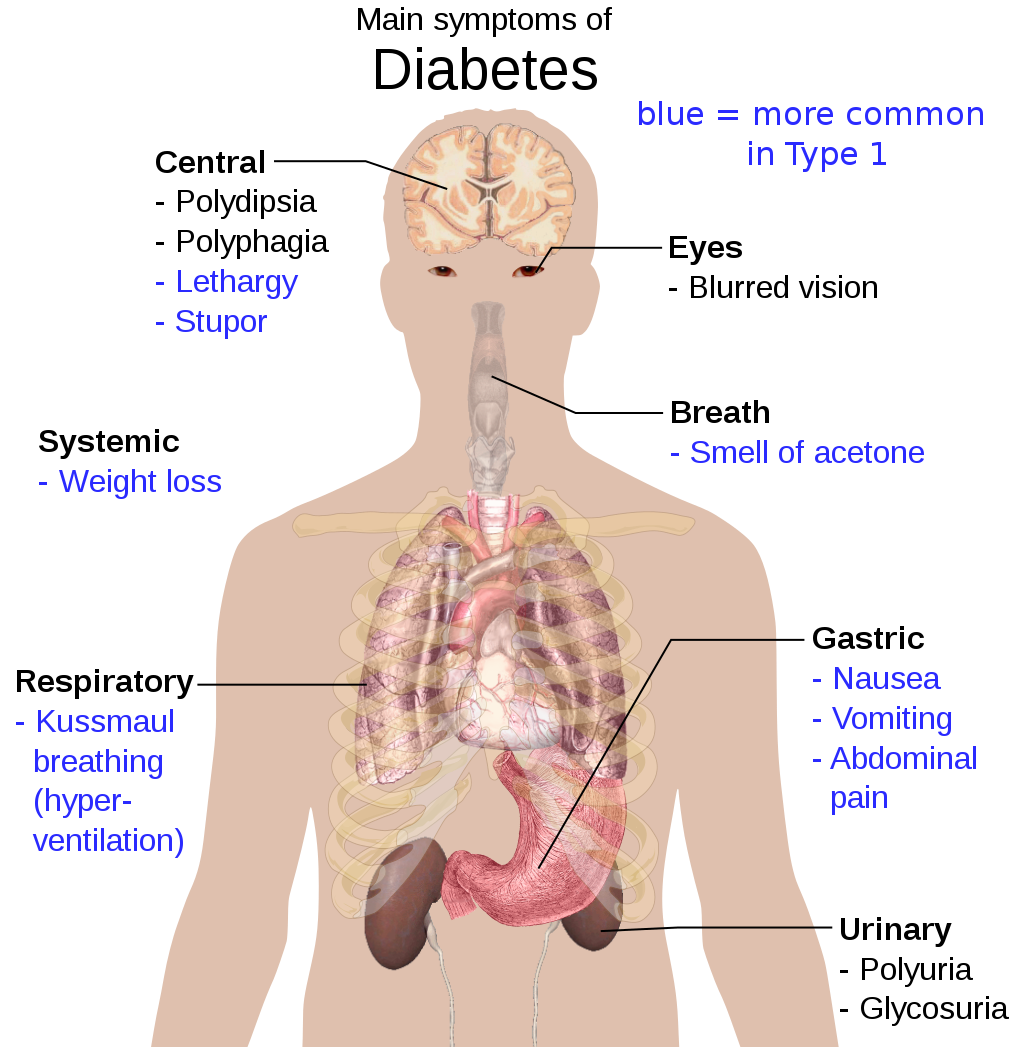
When diabetes is not well controlled, it is likely to have several serious long-term consequences. Most of these consequences are due to damage to small blood vessels caused by high glucose levels in the blood. Damage to blood vessels, in turn, may lead to increased risk of coronary artery disease and stroke. Damage to blood vessels in the retina of the eye can result in gradual vision loss and blindness. Damage to blood vessels in the kidneys can lead to chronic kidney disease, sometimes requiring dialysis or kidney transplant. Long-term consequences of diabetes may also include damage to the nerves of the body, known as diabetic neuropathy. In fact, this is the most common complication of diabetes. Symptoms of diabetic neuropathy may include numbness, tingling, and pain in the extremities.
Type 1 Diabetes
Type 1 diabetes is a chronic autoimmune disorder in which the immune system attacks the insulin-secreting beta cells of the pancreas. As a result, people with type 1 diabetes lack the insulin needed to keep blood glucose levels within the normal range. Type 1 diabetes may develop in people of any age, but is most often diagnosed before adulthood. For type 1 diabetics, insulin injections are critical for survival.
Type 2 Diabetes
Type 2 diabetes is the single most common form of diabetes. The cause of high blood glucose in this form of diabetes usually includes a combination of insulin resistance and impaired insulin secretion. Both genetic and environmental factors play roles in the development of type 2 diabetes. Type 2 diabetes can be managed with changes in diet and physical activity, which may increase insulin sensitivity and help reduce blood glucose levels to normal ranges. Medications may also be used as part of the treatment, as may insulin injections.
Feature: Human Biology in the News
Some patients with type 1 diabetes have been given pancreatic islet cells transplants from other human donors. If the transplanted cells are not rejected by the recipient’s immune system, they can cure the patient of diabetes. However, because of a shortage of appropriate human donors, only about one thousand such surgeries have been performed over the past ten years.
In June of 2016, a research team led by Dr. David K.C. Cooper at the Thomas E. Starzl Transplantation Institute in Pittsburgh, Pennsylvania, reported on their work developing pig islet cells for transplant into human diabetes patients. The researchers genetically engineered the pig islet cells to be protected from the human immune response. As a result, patients receiving the transplanted cells would require only minimal suppression of their immune system after the surgery. The pig islet cells would also be less likely to transmit pathogenic agents, because the animals could be raised in a controlled environment.
The researchers have successfully transplanted the pig islet cells into monkey models of type 1 diabetes. As of June 2016, the scientists were looking for funding to undertake clinical trials in humans with type 1 diabetes. Dr. Cooper predicted then that if the human trials go as well as expected, the pig islet cells could be available for curing patients in as little as two years.
9.7 Summary
- The pancreas is a gland located in the upper left abdomen behind the stomach that functions as both an endocrine gland and an exocrine gland. As an endocrine gland, the pancreas releases hormones (such as insulin) directly into the bloodstream. As an exocrine gland, the pancreas releases digestive enzymes into ducts that carry them to the gastrointestinal tract.
- Tissues in the pancreas that have an endocrine role exist as clusters of cells called pancreatic islets. The islets consist of four main types of cells, each of which secretes a different endocrine hormone. Alpha (α) cells secrete glucagon, beta (β) cells secrete insulin, delta (δ) cells secrete somatostatin, and gamma (γ) cells secrete pancreatic polypeptide.
- The endocrine hormones secreted by the pancreatic islets all play a role, either directly or indirectly, in glucose metabolism and homeostasis of blood glucose levels. For example, insulin stimulates the uptake of glucose by cells and decreases the level of glucose in the blood, whereas glucagon stimulates the conversion of glycogen to glucose and increases the level of glucose in the blood.
- Disorders of the pancreas include pancreatitis, pancreatic cancer, and diabetes mellitus. Pancreatitis is painful inflammation of the pancreas that has many possible causes. Pancreatic cancer of the endocrine tissues is rare, but increasing in frequency. It is generally discovered too late to cure surgically. Smoking is a major risk factor for pancreatic cancer.
- Diabetes mellitus is the most common type of pancreatic disorder. In diabetes, inadequate activity of insulin results in high blood levels of glucose. Type 1 diabetes is a chronic autoimmune disorder in which the immune system attacks the insulin-secreting beta cells of the pancreas. Type 2 diabetes is usually caused by a combination of insulin resistance and impaired insulin secretion due to a variety of environmental and genetic factors.
9.7 Review Questions
- Describe the structure and location of the pancreas.
- Distinguish between the endocrine and exocrine functions of the pancreas.
-
-
- What is pancreatitis? What are possible causes and effects of pancreatitis?
- Describe the incidence, prognosis, and risk factors of cancer of the endocrine tissues of the pancreas.
- Compare and contrast type 1 and type 2 diabetes.
- If the alpha islet cells of the pancreas were damaged to the point that they no longer functioned, how would this affect blood glucose levels? Assume that no outside regulation of this system is occurring and explain your answer. Further, would administration of insulin be more likely to help or hurt this condition? Explain your answer.
- Explain why diabetes causes excessive thirst.
9.7 Explore More
What does the pancreas do? – Emma Bryce, TED-Ed, 2015.
Type 2 diabetes in children, Children’s Health, 2008.
Reversing Type 2 diabetes starts with ignoring the guidelines | Sarah Hallberg | TEDxPurdueU, TEDx Talks, 2015.
Attributions
Figure 9.7.1
Insulin_Application by Mr Hyde at Czech Wikipedia (Original text: moje foto) on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 9.7.2
Blausen_0699_PancreasAnatomy2 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 9.7.3
Exocrine_and_Endocrine_Pancreas by OpenStax College is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0/deed.en) license.
Figure 9.7.4
Jaundice_eye_new by Info-farmer on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Original image, File:Jaundice eye.jpg, is from Centers for Disease Control and Prevention‘s Public Health Image Library (PHIL), with identification number #2860)
Figure 9.7.5
Main_symptoms_of_diabetes.svg by Mikael Häggström on Wikimedia Commons is released into the public domain (https://en.wikipedia.org/wiki/Public_domain).
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, July 19). Figure 23.26 Exocrine and endocrine pancreas [digital image]. In Anatomy and Physiology (Section 23.6). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/23-6-accessory-organs-in-digestion-the-liver-pancreas-and-gallbladder
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Children’s Health. (2008, June 13). Type 2 diabetes in children. YouTube. https://www.youtube.com/watch?v=qlzLSbAGMqA&feature=youtu.be
, , , , , , . (2016, March 4). First update of the International Xenotransplantation Association consensus statement on conditions for undertaking clinical trials of porcine islet products in type 1 diabetes—Executive summary. Xenotransplantation 2016, 23: 3– 13. https://doi.org/10.1111/xen.12231
TED-Ed. (2015, February 19). What does the pancreas do? – Emma Bryce. YouTube. https://www.youtube.com/watch?v=8dgoeYPoE-0&feature=youtu.be
TEDx Talks. (2015, May 4). Reversing Type 2 diabetes starts with ignoring the guidelines | Sarah Hallberg | TEDxPurdueU. YouTube. https://www.youtube.com/watch?v=da1vvigy5tQ&feature=youtu.be
A disease caused by problems with the pancreatic hormone insulin, which leads to high blood glucose levels and symptoms such as excessive thirst and urination; includes type 1 and type 2 diabetes.
A long, flat gland that sits tucked behind the stomach in the upper abdomen. The pancreas produces enzymes that help digestion and hormones that help regulate the way your body processes sugar (glucose).
One of millions of clusters of cells in the pancreas that secrete endocrine hormones such as insulin and glucagon; also called islet of Langerhans.
The smallest type of blood vessel that connects arterioles and venules and that transfers substances between blood and tissues.
Glucose (also called dextrose) is a simple sugar with the molecular formula C6H12O6. Glucose is the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, using energy from sunlight.
The chemical processes that occur in a living organism to sustain life.
A peptide hormone, produced by alpha cells of the pancreas. It works to raise the concentration of glucose and fatty acids in the bloodstream, and is considered to be the main catabolic hormone of the body. It is also used as a medication to treat a number of health conditions.
A hormone made by the pancreas that allows your body to use sugar (glucose) from carbohydrates in the food that you eat for energy or to store glucose for future use.
An endocrine hormone that inhibits the production of growth hormone by the pituitary and the secretion of insulin and glucagon by the pancreas, in addition to other functions.
A non-steroid hormone which helps the pancreas self-regulate secretion.
A painful inflammation of the pancreas due to gallstones, chronic alcohol use, or other cause.
Gland such as a sweat gland, salivary gland, or mammary gland that secretes a substance into a duct that carries the secretion to the outside of the body.
A disorder in which blood sugar (glucose) levels are abnormally high because the body does not produce enough insulin to meet its needs.
An autoimmune disorder in which the immune system destroys insulin-secreting beta cells in the pancreas, leading to loss of glucose control and high levels of blood glucose.
A multifactorial disorder in which a combination of insulin resistance and impaired insulin production lead to loss of glucose control and high levels of blood glucose.
A layer at the back of the eyeball containing cells that are sensitive to light and that trigger nerve impulses that pass via the optic nerve to the brain, where a visual image is formed.
Any gland of the endocrine system, which is the system of glands that releases hormones directly into the blood.
The ability of an organism to maintain constant internal conditions despite external changes.
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.

